|
Today – 27th February, 2019 – the long-awaited results of the Phase II GDNF clinical trial were published. GDNF (or glial cell line-derived neurotrophic factor) is a protein that our bodies naturally produce to nurture and support cells. Extensive preclinical research suggested that this protein was particularly supportive of dopamine neurons – a group of cells in the brain that are affected by Parkinson’s. The results of the Phase II clinical trial suggest that the treatment was having an effect in the brain (based on imaging data), but the clinic-based methods of assessment indicated no significant effect between the treatment and placebo groups. In today’s post we will look at what GDNF is, review the previous research on the protein, discuss the results of the latest study, and look at what happens next. And be warned this is going to be a long post!
|
 Boulder, Colorado. Source: Rps
Boulder, Colorado. Source: Rps
It all began way back in 1991.
George H. W. Bush was half way into his presidency, a rock band called Nirvana released their second album (‘Nevermind’), Michael Jordan and the Chicago Bulls rolled over the LA Lakers to win the NBA championship, and Arnold Schwarzenegger’s ‘Terminator 2’ was the top grossing movie of the year.
 Source: Stmed
Source: Stmed
But in the city of Boulder (Colorado), a discovery was being made that would change Parkinson’s research forever.
In 1991, Dr Leu-Fen Lin and Dr Frank Collins – both research scientists at a small biotech company called Synergen, isolated a protein that they called glial cell-derived neurotrophic factor, or GDNF.
And in 1993, they shared their discovery with the world in this publication:
 Title: GDNF: a glial cell line-derived neurotrophic factor for midbrain dopaminergic neurons.
Title: GDNF: a glial cell line-derived neurotrophic factor for midbrain dopaminergic neurons.
Authors: Lin LF, Doherty DH, Lile JD, Bektesh S, Collins F.
Journal: Science, 1993 May 21;260(5111):1130-2.
PMID: 8493557
For the uninitiated among you, when future historians write the full history of Parkinson’s, there will be no greater saga than GDNF.
In fact, in the full history of medicine, there are few experimental treatments that people get more excited, divided, impassioned and evangelical than GDNF.
This ‘wonder drug’ has been on a rollercoaster ride of a journey.
What exactly is GDNF?
GDNF stands for glial cell-derived neurotrophic factor.
Let’s break that down.
Glial cells are the support cells in the brain. While neurons are considered to be the ‘work horses’ of neurological function – passsing messages and storing memories – glial cells are in the background making sure that neurons are supported, protected and nurtured.
There are different types of glial cells, including astrocytes, oligodendrocytes and microglia. And each type has a specific function, for example microglia are the brain’s resident immune cells checking up on the health of the neurons while oligodendrocytes provide the neurons with a protective covering (called myelin sheath) which also helps to speed up the signalling of neurons.
 Different types of cells in the brain. Source: Dreamstime
Different types of cells in the brain. Source: Dreamstime
Astrocytes provide nutrients to neurons and make sure the environment surrounding the neurons is balanced and supportive. Glial cells are absolutely critical to the normal functioning of the brain.
So that is the “glial cell” part of glial cell-derived neurotrophic factor, now let’s focus on the latter part.
Neurotrophic factors (neurotrophic = Greek: neuron – nerve; trophikós – pertaining to food/to feed) are chemicals that nurture neurons and support growth. There are many types of neurotrophic factors, some having more beneficial effects on certain types of neurons and not other. GDNF is one of these neurotrophic factors.
Dr Leu-Fen Lin and Dr Frank Collins (who I mentioned above) isolated GDNF from a cell culture of rat glial cells – hence the name: glial cell-derived neurotrophic factor.
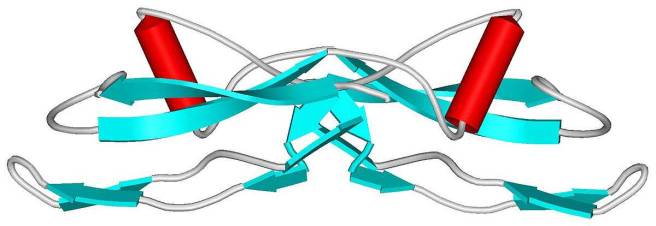 The structure of GDNF protein. Source: Wikipedia
The structure of GDNF protein. Source: Wikipedia
GDNF is a member of a larger family of neurotrophic factors.
And there are three other members of that family (called neurturin, persephin, and artemin – sounds like the Three Musketeers!) have also demonstrated positive effects on dying dopamine neurons. The positive/neuroprotective effect of these neurotrophic factors works via a series of ‘receptors’ on the outer surface of cells. Receptors are molecules sitting on the surface of cells, waiting for specific proteins to come along and bind to them. By binding to them, the receptor becomes activated.
There are receptors that are specific for each of the GDNF family members, and when they bind to their respective receptor, they activate another surface protein called RET.
 The GDNF family photo. Source: Nature
The GDNF family photo. Source: Nature
Ret proto-oncogene (or RET) is a receptor tyrosine kinase, that is a cell-surface molecule that initiates signals inside the cell after surface receptors are bound. The activation of RET results in cell growth and survival. Dopamine neurons in our brains have most of the GDNF family receptors and a lot of RET.
GDNF has its neuroprotective effect on dopamine neurons by activating its receptor, which activates RET (Click here for a very good OPEN ACCESS review of GDNF biology).
How much research has been conducted on GDNF in Parkinson’s?
A LOT!
GDNF has to be one of the most researched compounds for potential therapeutic use in Parkinson’s, because so much of the early data that was generated was so impressive.
[And this is where the roller coaster ride starts…]
One year after the original Lin and Collins GDNF report, the first reports of the neuroprotective properties of GDNF in animal models of Parkinson’s began to be reported (Click here, here and here for the first reports), and another year after that the first report of beneficial effects in non-human primate models of Parkinson’s were published (Click here to read more about this).
And it’s important to understand that these results have been independently replicated many, many times (Click here, here and here for some early examples). There is a great deal of research investigating all aspects of GDNF in models of Parkinson’s (Click here to read a good OPEN ACESS review of this topic).
[…the rollercoaster was heading up to lofty heights…]
As a result of all this positive data, a lot of members of the Parkinson’s research community got very excited that perhaps Dr Lin and Dr Collins had stumbled upon the much sought after “miracle cure” for Parkinson’s.
In 1994, the biotech company Synergen was immediately swallowed up by the Pharmaceutical company Amgen, which subsequently owned the rights to GDNF and its use in Parkinson’s.
Sensing that they were on to a potentially blockbuster treatment for Parkinson’s, Amgen quickly started setting up clinical trials to evaluated whether the neuroprotective effects of GDNF would translate into humans. Between July 1996 and April 1999, 50 people with advanced Parkinson’s had tubes implanted in their heads which accessed the ventricular system of the brain.
The ventricular system is space surrounding (and within) your brain that is filled with cerebrospinal fluid – the nurturing liquid that your brain sits in.
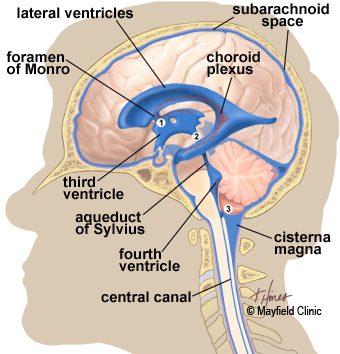 The ventricular system of the brain. Source: Mayfieldclinic
The ventricular system of the brain. Source: Mayfieldclinic
By putting the tube into the ventricular system and then injecting GDNF, the Amgen researchers were hoping that the GDNF would permeate and spread through the brain and find its way to the dopamine neurons.
Unfortunately, GDNF can not be given orally because it does not cross the blood brain barrier – a protective membrane surrounding the brain. But the results of the ventricular delivery approach suggested that this was not an ideal method of treatment:

Title: Randomized, double-blind trial of glial cell line-derived neurotrophic factor (GDNF) in PD.
Authors: Nutt JG, Burchiel KJ, Comella CL, Jankovic J, Lang AE, Laws ER Jr, Lozano AM, Penn RD, Simpson RK Jr, Stacy M, Wooten GF; ICV GDNF Study Group.
Journal: Neurology. 2003 Jan 14;60(1):69-73.
PMID: 12525720
The ventricular route of administration was flawed because the GDNF could not penetrate very deep into the brain, and as a result it had a very limited effect. Worse still because the cerebrospinal fluid provides access to the spinal cord and other regions of the central nervous system, numerous side effects were reported in the 38 study participants who received GDNF, including hyponatremia, nausea, vomiting, and paresthesias (prickly feeling in peripheral nerves).
The side effects led Amgen to halt the study prematurely – and unfortunately, it would not be the last time that Amgen would halt a GDNF trial.
[The GDNF rollercoast is crashing down from those initial giddy heights]
At this point, Amgen apparently shelved the drug. To their credit though, the company did make GDNF readily available to researchers seeking to work with it, but it would be another two years before any other humans were injected with it.
So what happened next?
During those years, Amgen was approached by multiple groups of researchers who were interested in conducting a clinical trial of GDNF in Parkinson’s, and the company finally agreed to supply the drug to a research team at the Frenchay Hospital in Bristol (UK).
 Bristol. Source: Megabus
Bristol. Source: Megabus
In this small clinical study, the GDNF was injected directly into the brain, into an area called the putamen. Dopamine neurons in the brain reside in an area called the substantia nigra, near the base of the brain, but they project their branches (or axons) to the several other areas, including the putamen, and this is where they release most of their dopamine.
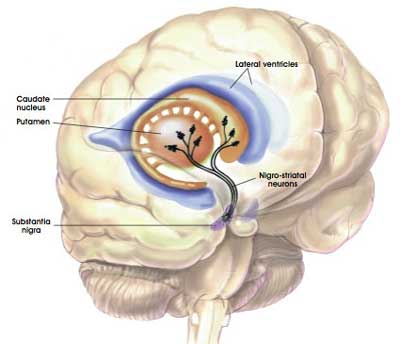 The projections of the substantia nigra dopamine neurons & location of the putamen. Source: MyBrainNotes
The projections of the substantia nigra dopamine neurons & location of the putamen. Source: MyBrainNotes
Appreciating that the putamen is where many of the branches of the dopamine neurons can be found, the researchers in Bristol hoped that by delivering GDNF to that region they would encourage the dopamine neurons to grow more branches. An example of regenerative medicine. They recruited 5 individuals with advanced Parkinson’s and implanted tiny tubes into the putamen, which would allow for the GDNF to be pumped into that region.
And what did the results of this trial find?
The results of this small Phase I study were rather remarkable.
[The rollercoast is pulling out of the dip and heading up again]
And they shocked the Parkinson’s research world when they were published in 2003:
 Title: Direct brain infusion of glial cell line-derived neurotrophic factor in Parkinson disease.
Title: Direct brain infusion of glial cell line-derived neurotrophic factor in Parkinson disease.
Authors: Gill SS, Patel NK, Hotton GR, O’Sullivan K, McCarter R, Bunnage M, Brooks DJ, Svendsen CN, Heywood P.
Journal: Nat Med. 2003 May;9(5):589-95.
PMID: 12669033
In this study, the researchers treated the 5 participants with GDNF for one year. The findings of the study found that GDNF treatment resulted in:
- a 39% improvement in the OFF-medication motor ability (according to the Unified Parkinson’s Disease Rating Scale (UPDRS))
- a 61% improvement in how subjects perceived their ability to go about daily activities.
- a 64% reduction in medication-induced dyskinesias (and they were not observed off medication)
- no serious clinical side effects (none of the issues reported in the first study)
Importantly, the researchers conducted brain imaging studies on these participants and they reported a 28% increase in striatum dopamine storage after 18 months (based on Fluorodopa PET scans).
And then of course, there are the videos.
The videos?
This is a video of some of the patients involved in the first pilot study of GDNF. As you will see, the difference between the before and after footage is rather striking:
(If you have sound on, you can hear Tom Isaacs and Dr Stephen Gill talking about GDNF)
And the effect of the GDNF treatment appeared to have long lasting effects in these individuals, as a two year follow-up study suggested:
 Title: Intraputamenal infusion of glial cell line-derived neurotrophic factor in PD: a two-year outcome study.
Title: Intraputamenal infusion of glial cell line-derived neurotrophic factor in PD: a two-year outcome study.
Authors: Patel NK, Bunnage M, Plaha P, Svendsen CN, Heywood P, Gill SS.
Journal: Ann Neurol. 2005 Feb;57(2):298-302.
PMID: 15668979
In this study, the same 5 patients demonstrated a 57% and 63% improvement in their OFF-medication motor and activities of daily living subscores (Unified Parkinson’s Disease Rating Scale) after 2 years of treatment.
And the researchers also published a case study of one trial patient, suggesting that the positive effects of GDNF were still having an impact 3 years after the drug had stopped being delivered (Click here to read more about that report). There was also a postmortem analysis of one participants brain indicating the sprouting of dopamine fibres in the putamen (Click here for more on this).
This is amazing! So what happened next?
[The rollercoast is racing up to another peak… I wonder what could come next?]
There was one major issues with the Phase I GDNF clinical study: the trial was an open label.
Both the participants taking part in the study and the physicians conducting the study knew who was getting the drug. The study was not blind, which opens the door to the potential for a major placebo effect (more on this below).
An independent replication of the study was required and that came in 2007:
 Title: Unilateral intraputamenal glial cell line-derived neurotrophic factor in patients with Parkinson disease: response to 1 year of treatment and 1 year of withdrawal
Title: Unilateral intraputamenal glial cell line-derived neurotrophic factor in patients with Parkinson disease: response to 1 year of treatment and 1 year of withdrawal
Authors: Slevin JT, Gash DM, Smith CD, Gerhardt GA, Kryscio R, Chebrolu H, Walton A, Wagner R, Young AB.
Journal: J Neurosurg. 2007 Apr;106(4):614-20.
PMID: 17432712
In this Phase I study, 10 people with Parkinson’s were unilaterally implanted with a tube to deliver GDNF to the putamen. This means that only one side of the brain was being treated with GDNF. But after 12 months of treatment, the participants had improved by 42 and 38% in the OFF- and ON-medication states according to the total UPDRS score.
[Be warned, the rollercoaster is peaking here]
After 12 months of treatment, the participants were taken off the GDNF (the sponsor deliberately stopped the treatment based on other events – see below), but they were assessed for another 12 months. The benefits from the GDNF treatment were completely lost by 9 to 12 months after stopping the GDNF infusion (the UPDRS scores had returned to their baseline levels).
[Rollercoaster is discovering gravity again, and heading for another dip…]
More importantly, 7 of the 10 participants had apparently developed antibodies to GDNF.
What are antibodies?
Antibodies are Y-shaped proteins that the immune system naturally and continuously produces to identify anything in the body that is ‘not self’ (that is, not a normally occurring part of you – think of viruses, bacteria, etc).

Monoclonal antibodies. Source: Astrazeneca
Antibodies act like alert flags for the immune system.
When antibodies bind to something, they alert the immune system to investigate and potentially remove. The binding of an antibody to a protein can also prevent the protein from doing its function. Thankfully, this development did not result in an immune reaction in any of the participants, which could have resulted in the body attacking any source of GDNF – foreign or self.
This doesn’t sound like a good development though. What happened next?
[Gravity has hold of the Rollercoaster…]
In parallel to this small Phase I study, Amgen also initiated a double blind clinical trial for GDNF with 34 participants. Being double blind, both the researchers and the participants did not know who was getting GDNF or a control treatment. The procedure used a very different pump to deliver the GDNF into the brain (compared to the one used in the Bristol study), and some have suggested that this may have contributed to the outcome of this study.
What was the outcome of that study?
In June 2004, Amgen announced that its clinical trial testing the efficacy of GDNF in treating advanced Parkinson’s had shown a biological effect (based on Fluorodopa PET brain imaging), but failed to demonstrate any clinical improvement (compared to placebo treatment) after six months of use (Click here to read the press release).
[…and the rollercoaster is now in free fall…]
Later that year (in September), Amgen halted the study completely. They cited two reasons:
- Pre-clinical data from non-human primates that had been treated in the highest dosage group for six months (followed by a three-month washout period) exhibited a significant loss of neurons in an area of the brain called the cerebellum (which is involved in coordinating movement)
- They had detected antibodies in 18 of the 34 study participants (4 of whom had developed neutralising activity – Click here to read more about this).
The results of this study were published in 2006:
 Title: Randomized controlled trial of intraputamenal glial cell line-derived neurotrophic factor infusion in Parkinson disease.
Title: Randomized controlled trial of intraputamenal glial cell line-derived neurotrophic factor infusion in Parkinson disease.
Authors: Lang AE, Gill S, Patel NK, Lozano A, Nutt JG, Penn R, Brooks DJ, Hotton G, Moro E, Heywood P, Brodsky MA, Burchiel K, Kelly P, Dalvi A, Scott B, Stacy M, Turner D, Wooten VG, Elias WJ, Laws ER, Dhawan V, Stoessl AJ, Matcham J, Coffey RJ, Traub M.
Journal: Ann Neurol. 2006 Mar;59(3):459-66.
PMID: 16429411
What followed was an ugly chapter in the story of GDNF.
Amgen refused to allow their study participants to continue to use GDNF when they requested it on compassionate use grounds. Lawyers then got involved (two lawsuits in 2005), but the judges decided in favour of Amgen.
[…still falling]
As all of this was going on, other members of the GDNF neurotrophic factor family were being tested in models of Parkinson’s, particularly Neurturin. Much of this research used a different form of delivery – called gene therapy.
What is gene therapy?
Gene therapy is an experimental treatment approach that involves treating Parkinson’s with DNA rather than drugs.
The gene therapy involves inserting a piece (or multiple pieces) of DNA into a cell which will cause the cell to start to produce proteins that they usually do not. The introduction of the DNA is usually achieved using genetically modified viruses which have had all the disease causing component removed, allowing us to use the virus as an efficient delivery system. Viruses by their very nature are good at infecting cells so if we remove the disease causing components, what is left is a very efficient biological delivery system.
 Gene therapy. Source: Yourgenome
Gene therapy. Source: Yourgenome
[Could the rollercoaster be showing signs of going up again?]
A biotech company called Ceregene was at the leading edge of this approach and they initiated clinical trials of their gene therapy product called CERE-120.
 The Phase I study suggested that the treatment was safe and well tolerated (Click here to read more about this), so the company initiated a Phase II clinical trial (Click here to read the details of that study), and the results were published in 2012 (Click here to read those) with a longer-term follow up set of results being published in 2015:
The Phase I study suggested that the treatment was safe and well tolerated (Click here to read more about this), so the company initiated a Phase II clinical trial (Click here to read the details of that study), and the results were published in 2012 (Click here to read those) with a longer-term follow up set of results being published in 2015:
 Title: Gene delivery of neurturin to putamen and substantia nigra in Parkinson disease: A double-blind, randomized, controlled trial
Title: Gene delivery of neurturin to putamen and substantia nigra in Parkinson disease: A double-blind, randomized, controlled trial
Authors: Warren Olanow C, Bartus RT, Baumann TL, Factor S, Boulis N, Stacy M, Turner DA, Marks W, Larson P, Starr PA, Jankovic J, Simpson R, Watts R, Guthrie B, Poston K, Henderson JM, Stern M, Baltuch G, Goetz CG, Herzog C, Kordower JH, Alterman R, Lozano AM, Lang AE.
Journal: Ann Neurol. 2015 Aug;78(2):248-57.
PMID: 26061140
In this study, between December 2006 and November 2008, 58 patients at 9 research sites across the USA were recruited to the trial. The participants were randomly assigned to either receive bi-lateral injections in the brain of an AAV-virus containing the DNA of neurturin, or a shame surgery. But after a 15- to 24-month study, the investigators found no difference between the participants.
All of these developments (and more) left many in the Parkinson’s research community thinking that neurotrophic factors were not going to work for this condition.
[The brakes have been applied and the rollercoaster has come to a complete stop at the bottom of the dip]
And perhaps, the situation would have remained like this, if not for the dogged efforts of certain inidividuals who brought about the Phase II Bristol GDNF clinical trial.
Who were these ‘dogged’ individuals?
One of them was Tom Isaacs.
In 1996 – at just 27-years of age – Tom, a London-based surveyor, was diagnosed with Parkinson’s. After dealing with the initial shock of it all, Tom embraced his situation and became a committed, (utterly) tireless activist. He firstly walked the entire coastline of the UK to raise money and awareness for Parkinson’s.

His book, “Shake well before use“, discusses that trip and adapting to life with Parkinson’s (it is a fantastic read). Half way through his epic walk, however, the Phase I GDNF clinical trial results were published and caused a sensation. Tom was told by a friend: “You can stop walking, they have cured it”
Tom completed his walk though and upon returning to London, he (along with three others) founded and set up the Cure Parkinson’s Trust. He was a passionate advocate for GDNF and one of the driving forces behind the Phase II Bristol GDNF trial.
Another enthusiastic proponent of the GDNF approach was Prof Stephen Gill, who was the lead investigator on the Phase I clinical study which provided the original GDNF results. Prof Gill was also the inventor of the innovative delivery system used in the clinical trials.
 Prof Steven Gill. Source: Spire
Prof Steven Gill. Source: Spire
Amusing anecdote – the first time Tom Isaacs met Prof Gill was during his 2002 coastal walk as Tom was passing by Bristol. After crossing the Severn bridge, they met at the Severn View service station, bought a cup of coffee, sat down and talked about GDNF.
 The Severn View service station. Source: Geograph
The Severn View service station. Source: Geograph
A third character that deserves mention in the story of the Bristol GDNF Phase II clinical trial is Bryn Williams, founder of Funding Neuro – a charity focused on funding research that will accelerate the cures for neurological conditions. Bryn has been a passionate advocate for the Bristol GDNF clinical trial.
 Bryn Williams. Source: Herald
Bryn Williams. Source: Herald
So what was the Bristol GDNF trial?
In January 2010, while the gene therapy clinical trials were being conducted for neurotrophic factors, Amgen licenced the rights to GDNF to a company called Medgenesis.
 And the folks at Medgenesis were very keen to see another clinical trial in Parkinson’s
And the folks at Medgenesis were very keen to see another clinical trial in Parkinson’s
Together with the Cure Parkinson’s Trust & Bryn Williams, Prof Gill approached Parkinson’s UK and proposed conducting another Phase II double blind clinical study of GDNF in individuals with advanced Parkinson’s.
Parkinson’s UK agreed that it was a good idea and also agreed to fund the bulk of the study.
The new study began in 2012, and it involved a revolutionary new method of delivering the treatment, which involved tubes being implanted in the brain with pin point precision thanks to the assistance of robotics (a system developed by Prof Gill and a company called Renishaw). These tubes connected with another tube which ran to a small port which was placed just behind the ear.
 Source: Medium (a very good article from Parkinson’s UK discussing the study)
Source: Medium (a very good article from Parkinson’s UK discussing the study)
And it was via this port that the GDNF (or placebo) treatment was delivered to the participants in the study.
 A participant receiving treatment. Source: Parkinson’s UK
A participant receiving treatment. Source: Parkinson’s UK
I am often referring to “added value” being an important part of any future clinical trials, and this delivery system is a fantastic example of this. This same technology is now being used in the ongoing CDNF clinical trial for Parkinson’s being conducted in Finland/Sweden (more on this below) as well as multiple oncology clinical trials. Regards of the results of the GDNF trial, the output of the study has already had tremendous benefits (‘added value’) for the wider medical community.
Sounds very interesting. So the results of the study were published today?
Yes, in the prestigious journal ‘Brain’:
 Title: Randomized trial of intermittent intraputamenal glial cell line-derived neurotrophic factor in Parkinson’s disease
Title: Randomized trial of intermittent intraputamenal glial cell line-derived neurotrophic factor in Parkinson’s disease
Authors: Whone A, Luz M, Boca M, Woolley M, Mooney L, Dharia S, Broadfoot J, Cronin D, Schroers C, Barua NU, Longpre L, Barclay CL, Boiko C, Johnson GA, Fibiger HC, Harrison R, Lewis O, Pritchard G, Howell M, Irving C, Johnson D, Kinch S, Marshall C, Lawrence AD, Blinder S, Sossi V, Stoessl AJ, Skinner P, Mohr E, Gill SS.
Journal: Brain, 2019: 142; 512–525
PMID: 30808022 (This report is OPEN ACCESS if you would like to read it)
In this study, the researchers began by screening individuals to identify those appropriate for the study. Between October 2012 and April 2015, 196 inidividuals from throughout the UK were screened. Of these, 41 individuals were selected to take part in the study. The investigators began the study with a small pilot group of participants (6 people) to assess the safety of the surgical technique and the administration of the GDNF. Once optimised, the remaining 35 participants were given the surgical procedure. All of the participants were then randomised and treated for 40 weeks with either GDNF or the placebo treatment (Click here to read more about the details of the trial).
The primary endpoint of this trial was the percentage of change from the baseline measure in the practically-defined OFF state UPDRS motor score (part III) after 40 weeks of double-blind treatment. This means, how the degree of improvement in participants when they are not on their medication, between the start of the study and the end of the study. Clinical assessments were conducted at the baseline, 8 weeks, 16 weeks, 24 weeks, 32 weeks, and 40 weeks timepoints.
The secondary endpoints of the study included:
- The percentage of change between baseline and the Weeks 40 timepoint in UPDRS motor score in the ON state (that is, the motor performance of participants while on medication)
- The percentage of change from baseline in UPDRS activities of daily living scores in the OFF and ON state
- The UPDRS parts I and IV scores
- The change between baseline to the Week 40 timepoint in Parkinson’s diary ratings.
In addition to these, numerous supplemental endpoints were also measured, including Fluorodopa brain imaging. The imaging was conducted at baseline (before treatment) and again at the 40 weeks timepoints.
The results of the study suggest that there was no difference in OFF or ON performance at the 40 week timepoint between the GDNF and placebo treated group. As you can see in the graph below, both group began improving soon after treatment began, and they both continued to do so across the 40 weeks of the study. A decrease in UPDRS score suggests an improvement in the motor performance of the participants, and both the red line (GDNF treatment) and the blue line (Placebo group) on the graph have a downward tragectory.
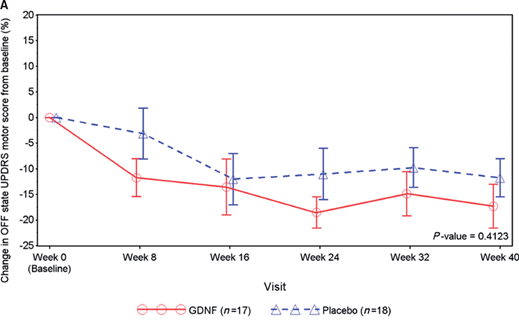 Source: Brain
Source: Brain
Admittedly, the red line is lower than the blue line, but this never gets statistically significant.
How do we explain this?
There may be a difference of opinions here, but I would lean towards a placebo response.
What is a placebo response?
A placebo response occurs when one exhibits a reaction to a treatment, for which there is no pharmacological reason. There is no biological reason why the placebo treatment caused the control group to improve, but they did.
In addition, none of the secondary endpoints exhibit any significant differences between the two groups.
This is really bad right?
It is unfortunate, but it is not the end of the world.
More importantly, there some very interesting findings in the overall results.
Such as?
The responders.
Que?
Every drug trial has individuals who respond better than anyone else in the study, and this study was no different. Some members of the GDNF treated group responded better than others to the treatment.
But crucially, this ‘responder difference’ points towards a difference between the GDNF and placebo group.
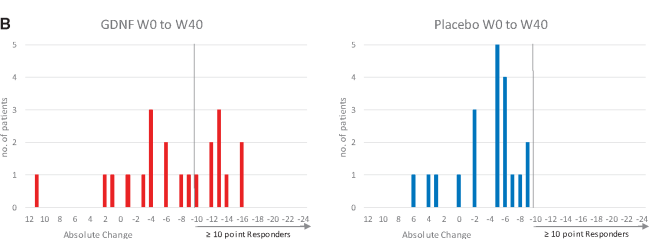
You see, when the researchers looked at number of participants who achieved a better than 10 point improvement on the OFF UPDRS score, there were 9 who experienced this in the GDNF group, but none in the placebo treated group. While there were many individuals who had a placebo response in the control/placebo group, none of them had a response as big as the GDNF responders.
And you can see this is the graphs below. On the left (GDNF treated group), there are 9 red bars beyond the >10 point responder line, but on the right (blue) side there are none.
 Source: Brain
Source: Brain
Interesting. Anything else of interest?
Yeah: The brain imaging results.
Have a look at the image below:
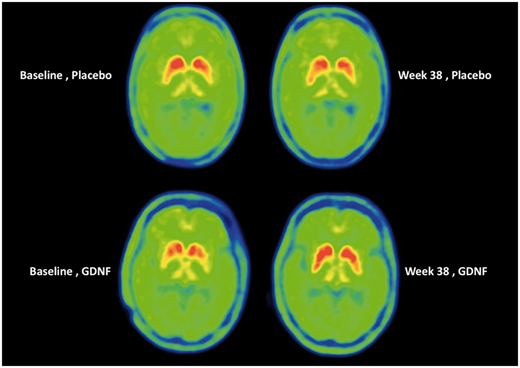 Source: Brain
Source: Brain
Each of the 4 green circles represents a birds-eye view of the brain. The red/yellow regions are the putamen on each side of the brain, and the greater the intensity of red colouration, the greater the level of dopamine activity. Now, if you look at the two brains in the top row, these are images from the same individual (baseline image on the left and 40 week image on the right). Note the subtle reduction in red colouration in the right (40 weeks) image compared to the left (baseline) image (particularly around the bottom tips of the putamen). This loss of red colouration suggests a reduction in dopamine activity. The images in the top row came from an individual who was treated with the placebo during the study.
Now shift your attention to the bottom row of brain images, and note the increase in red colouration in the right hand image (the 40 week timepoint). I hope you will agree that compared to the baseline image (left), there is a lot more red colouration on the 40 weeks (right) image. This difference suggests an increase in dopamine activity.
What could the brain imaging results mean?
It suggests that the GDNF was having a biological effect in the brain – the treatment was doing something. Exactly what that ‘something’ is still needs to be determined.
There are in effect three possible explanations:
1. There is an increase in dopamine turnover in the remaining dopamine fibres
2. There is an increase in the number of dopamine fibres
3. There is an increase in other types of neuronal fibres which can take up Levodopa
All three explanations are possible. But we currently have no means of testing which is the answer – beyond repeating the experiment with a larger range of brain imaging assessments.
But I hope you will agree that this is a very interesting part of the results and it certainly deserves further investigation.
Interesting. Anything else?
One other really interesting detail in the results: No antibodies.
Across both the double-blind and open label parts of the study, the researchers never detected any antibodies against GDNF in the analysed blood of participants at anytime during this study.
(NOTE: After the 40 weeks of double blind study, there was another 40 weeks of open label assessment in which all of the participants received GDNF – Click here to read the report on that phase of the study).
So what happens next?
Well, this does not appear to be the end of GDNF or neurotrophic therapy approaches for Parkinson’s.
There are a lot of ongoing discussion regarding whether there should be another trial to follow up the responder data and the brain imaging results. There are questions being asked as to whether the dose of GDNF was high enough to have an effect – the dose used was 3.5-fold smaller than in the historic continuous dosing studies (120 µg versus 420 µg), for safety reasons based on the neurodegenerative results from primates. In addition, some folks are asking if the study was long enough.
And while these discussion regarding GDNF continue, we should get some news soon about another neurotrophic factor clinical study which is using the same delivery system as the Bristol GDNF study. The cerebral dopamine neurotrophic factor (CDNF) clinical trial being conducted in Finland and Sweden is scheduled to finish this year, and we will hopfully get some news about that study. This study is being run by the biotech firm, Herantis.
 The Phase I/II study is evaluating the safety and tolerability of CDNF in people with Parkinson’s. Similar to the Phase II GDNF study, the drug is injected directly into the brain using an implanted canular system. One-third of the participants have received monthly infusions of placebo and two-third of the participants have received monthly infusions of either mid- or high-doses of CDNF for 6 months (Click here to read more about this trial). An extension study of this trial has recently been initiated (Click here to read more about that study).
The Phase I/II study is evaluating the safety and tolerability of CDNF in people with Parkinson’s. Similar to the Phase II GDNF study, the drug is injected directly into the brain using an implanted canular system. One-third of the participants have received monthly infusions of placebo and two-third of the participants have received monthly infusions of either mid- or high-doses of CDNF for 6 months (Click here to read more about this trial). An extension study of this trial has recently been initiated (Click here to read more about that study).
The topline results from this study will not be available until next year, but the safety/tolerability data from this trial are going to be presented the Alzheimer’s/Parkinson’s 2019 meeting in March. It will be interesting to see what those results suggest.
In addition to this study, there is a gene therapy GDNF clinical trial starting in California. This study was originally supposed to be conducted on the east coast of the US, but it has been shifted to the west coast, and it will hopefully be starting in the summer. This study will involve an AAV virus being injected into the brain, which will infect cells with the DNA required for the production of GDNF – causing cells in a particular region of the brain to start producing GDNF (Click here to learn more about this trial). We will be keeping an ear to the ground for information relating to this study.
And on top of this, there is also a company called Genecode, which is developing orally delivered “small molecules that mimic GDNF and trigger neurotrophic signalling in dopaminergic neurons” (Source). It will be interesting to see what happens with this company.
 Phew, Long post! So summing up. What does it all mean?
Phew, Long post! So summing up. What does it all mean?
Not just yet.
There is somethings else we really need to discuss.
There is no way of avoiding the fact that there was an enormous placebo response in the control/placebo-treated group in this study. As I mentioned above, a placebo response occurs when one exhibits a reaction to a treatment, for which there is no pharmacological reason. There was no biological reason why the placebo treated group should have improved, but they did.
Some folks might suggest that the surgical procedure instills a strong chance of placebo effect. Others will point towards the excellent and dedicated clinical care at a single research site (which was committed to maximising patient retention) possilby aiding this situation. While I am open to theories or ideas as to what could have caused the placebo response, I am biased towards a more human answer: This trial started with some mighty big expectations on the part of everyone involved (both the participants and the coordinators).
And this potential for a placebo response deeply concerns me as we start to put further resources towards large clinical trials for treatments that the community already has high expectations for (think: Exenatide). Placebo response is acknowledge as a problem in Parkinson’s (Click here to read an old SoPD post about this), and the Bristol GDNF study provides a fine example of it.
We need to have a careful think about managing expectations going forward.
So what does it all mean?
I hope I will be forgiven for using the rollercoaster analogy in this post, but I have watched the GDNF saga from the sidelines since starting my PhD in 2002. The lab I conducted my doctoral research in was one of many that produced some of the early preclinical GDNF data, so I was surrounded by the buzz of excitement about this amazing new compound. I have read the “Monkeys in the middle” book by Nick Nelson (a very good, but slightly dated review of the GDNF story), and I have followed every subsequent twist and turn of this tale.
I like to think that have provided a fair overview of the GDNF story and description of the latest clinical trial results in this post (and I am happy to be corrected on any details).
But please understand, there is a terrible sense of having been to this rodeo before.
Of having watched the rollercoaster do the loop-the-loop several times.
God all mighty, it’s deja vu all over again.
There are going to be lots of voices in the aftermath of these results being published, and my hope is that unlike many previous unsuccessful clinical trials which have been swept under the rug and forgotten (40% of Parkinson’s clinical studies do not publish their results – Click here for more on that rather damning statistic), I hope that the Bristol GDNF clinical trial will be the trigger for change.
An acknowledgement by the entire community that our clinical trial process needs to be carefully reconsidered and adapted. A very sober analysis of the Bristol GDNF study is required. It should involve voices from all sides of the clinical trial process. Patients, clinicians, everyone. A constructive conversation about how we can improve things and do better. Please let us learn from this experience, and use that knowledge to plan for better – and ideally more successful – future clinical trials.
EDITOR’S NOTE – The author of this post is an employee of the Cure Parkinson’s Trust and the President of his local Parkinson’s UK support branch. Both of these organisations – the Cure Parkinson’s Trust and Parkinson’s UK – funded the Bristol Phase II clinical trial of GDNF in Parkinson’s. Neither organisation nor the GDNF team at Bristol Hosptial have asked for this post to be written. This post has been provided by the author solely for the purpose of sharing what he considers to be an interesting story of medical research.
The banner for today’s post was sourced from the Cure Parkinson’s Trust




Thanks Simon for yet another great article.
There are a large number of statistics. One that interests me is the confounding role that the drug regimen plays in these results. See the paper by Whone et al..
The mean duration (Table 1) since original diagnosis is 8.6 years for the GDNF group and 7.9 years for the control group. Table 2 shows a levodopa equivalent daily dose for the GDNF group of 1019mg and 1026mg at baseline and at 40 weeks respectively, and for the placebo group of 978mg and 1077mg. The baseline values seem higher than I would expect for UK PwP at this stage in the disease. And, I note that while on average (but not individually) the drug regimen stayed the same for the GDNF group, it went up on average by almost 100mg/day for the placebo group. The increase in meds is likely to lead to improvements. This suggests to me that the true value of the placebo was less than that reported and, therefore, increasing the true value of the treatment.
Finally, we need to be careful in any post hoc analysis that we do with the data.
LikeLiked by 1 person
Hi John,
Thanks for your interesting comment. I thought the two groups were rather well balanced for a random allocation (compared to the Phase II exenatide baseline measures), but there is a lot intra-group variability, but that comes with such a small group. I too noticed the medication shift, but I doubt that this would impact OFF scores very much.I left dose details out of the post for the space/time sake – this post could have gone on forever, there are so many aspects to this that haven’t been touched on. And any post hoc analysis will be very difficult with such a small cohort, but it would be interesting to know if the 10 point+ responders in the GDNF group had any obvious differentiating characteristics. We shall see.
Kind regards,
Simon
LikeLike
Thanks as always Simon. And thanks to the brave participants.
What’s interesting is looking at the 80 week data. 10% of the participants had a 20 point or better improvement in off state UPDRS after 80 weeks! Is anyone going to continue to week 120?
Also interesting is th speculation that the surgery/injection may have initiated a response via the mechanical trauma. Hopefully it’s not just observer biased data.
As an engineer, it seems silly to define success or failure via an arguably arbitrary “endpoint” before the first data is ever taken. Yes we need to understand if there is placebo effect, and we need to be able to reproduce results, but science is all about setting up an experiment, interpreting the results and the deciding what to do next. Let’s separate ourselves from the fda’s burden of proof for awhile.
Does anyone know why acupuncture works? I’m not sure, but It does help with some conditions? Yes, and my insurance covers it…. What is the placebo control for hip surgery?
Great post and interesting data. Looking forward to where this goes next.
LikeLiked by 1 person
Hi Double,
Thanks for the very interesting comment. I didn’t do the second paper justice by leaving it out, but this post was getting crazy long so I drew the line. Plus being open label, the second 40 week phase of the second was open to bias so I am reluctant to take too much from that data beyond the treatment was safe long term and there were no antibodies. The trial was finished at 80 weeks and there was no further treatment (the company Medgenesis had very little GDNF left at that point) or follow up of the participants. It is a real shame that PET imaging was not taken at the 80 weeks time point, it would have been interesting to see any change in the placebo group and if there was further increases in the GDNF group, after both groups had a further 40 weeks of GDNF. But PET imaging is extremely expensive.
I am intrigued with the second half of your comment, particularly as we are entering a phase of clinical trialling now where UPDRS (primary outcome) might suggest no effect, and an added value measure (a secondary outcome – like a novel biomarker) might suggest a positive response – what does one do in such a scenerio? What do the regulators do? There is a lot of discussion within the research community about the usefulness of the clinical rating scales (is UPDRS right for the task?). One of the outcomes of this study will hopefully be a careful re-examination of this assessment process.
“Let’s separate ourselves from the fda’s burden of proof for awhile”. What would an engineer suggest? I am sincerely interested.
Kind regards,
Simon
LikeLike
“What would an engineer suggest? I am sincerely interested.”
Be careful what you ask for Simon, because you just might get a very opinionated earfull. Also this feedback is very “motor centric”
UDPRS is the best measure we have today, but it sucks…
-To start, when i go from a 0 to a 1 in UDPRS, i’ve already had the disease for 5-10 years?
-It’s a human attempt to try to project a linearized scale on a disease progression where we’re observing (not measuring) a third order result of the core issue (loss of dopamine translates to poor electrical signaling which translates to mechanical symptoms).
-Applying statistical analysis to establish efficacy over a placebo is sketchy given we have such a made up scale. Is going the from 30 to 40 the same as going from 20 to 30? Should stiffness be weighted more than tremor? Even stating % increase or decrease is a stretch. What does that even mean?
-Perhaps a better use of UDPRS would be for directionality. ie are people getting better or worst. What % of the data points were better than baseline? Better than placebo? I think we can agree better UDPRS translates to an improvement in disease severity.
-WE should also look at individual segments, not the whole UDPRS. How did stiffness compare between groups? between patients?
We need Biomarkers.
-CD4 count of cells per cubic mm is something you can apply a real statistical analysis to, because it is something you can really measure
-We should look at electrical signaling. There is nothing wrong with my muscles, but the signals going to them have issues. Yes the issues start in the brain, but i’ve seen very little on this. Why can’t we measure tremor in mVrms at the limb or look at signal slew rate as a measure of slowness or bradykinesia? These are more numbers you can apply a standard deviation to and know it’s going to make sense…
We should look at they outliers
-I’d love to talk to the people who got the most/least benefit. What is different about them?
-I don’t think anyone expects a magic bullet so we should assume not everyone will be helped when we establish enpoints.
Apologies for the typos… i have a neurological disorder that affects my ability to type. 🙂
LikeLiked by 1 person
Another thought on parsing the data. Given the treatment was localized literally with the location of injection, I wonder if the data could be parsed assuming location of improvements or lack of improvement. Ie did improvements in right arm testing (or upper extremity testing) improve dramatically over baseline or placebo? Why not do some 3D contour with subgroups of before and after?
Again, Finger taps+ foot stomps + facial expressions+ postural stability are quite difficult to add up.
1+dog=yellow
LikeLike
If placebo have such powerful impact continuously on motor skills, does anybody tried to investigate nature of it(MRI)? Possibly person can control brake kind of function if it’s own brain
LikeLiked by 1 person
Hear, hear Gk, while we are waiting for cure and better still prevention, it ould seem a good idea to work out how to activate a placebo effect. Is it maybe what is going on with exercise, PD warrior, Dance for PD, Parkinson Voice project and others that have great effect. At least we don’t have to wait for approval of a drug!
Eirwen
LikeLike
Hi Eirwen,
I agree that researching the mechanisms that activate the placebo effect could be greatly beneficial for improving how we treat Parkinson’s. Thankfully, there are a lot of researchers already exploring this.
Kind regards,
Simon
LikeLiked by 1 person
Hi GK,
Thanks for your comment. There is a joke in placebo research: A doctor hands a patient a prescription and say “I want you to take this placebo. If your condition doesn’t improve, I’ll prescribe you a stronger one”.
Yes, folks are researching placebo response in Parkinson’s (I think I’ll be writing a post on this in the not too distant future). This report here (https://www.ncbi.nlm.nih.gov/pubmed/18228568) for example is particularly interesting. It analysed data from 11 different PD trials and found that placebo response was associated with “higher baseline UPDRS scores and studies that focused on PD with motor fluctuations, surgical interventions, or those with a higher probability of placebo assignment” (which is basically the GDNF trial!). Researchers are also investigating the mechanims of the ‘placebo effect’ in order to better understand the biology of movement and other aspects of Parkinson’s (for example: https://www.nature.com/news/parkinson-s-patients-trained-to-respond-to-placebos-1.19341#/b1)
It would be great if we could just treat folks with some kind of ‘placebo effect’, but there is also something deeply unethical about such fakery – particularly in the case of progressive conditions like Parkinson’s, the mechanisms of which would still be continuing their course under the surface.
Kind regards,
Simon
LikeLike
Thanks Simon I will look forward to your post.
LikeLike
In DBS, patients can experience improvements “before switch on”. Could the placebo group not have experienced improvements as a result of the region of the brain being stimulated by the implant procedure, and ‘just’ the stimulation pumping the placebo in had on the brain?
LikeLiked by 2 people
Hi Andy,
Thanks for the really interesting question.
Yes, this is a possibility. There is a loop between where the dopamine neurons live (the substantia nigra) and the putamen. The dopamine neurons send branches to the putamen, and cells in the putamen send branches to the dopamine neurons. In Parkinson’s you lose the dopamine neurons to the putamen part of the loop, but preclinical models suggest that if you damage the other side of the loop (putamen cells to the dopamine neurons), you can see improvements in motor output.
Most DBS, however, are targeting other regions of the brain (such as the subthalamic nucleus) which are not directly involved with that loop I just mentioned. It could be that the damage caused by the implantation of the electrodes in DBS (or the tubes in the case od GDNF) could have a minor beneficial effect.
Kind regards,
Simon
LikeLike
Great work Simon.
Can we ever describe treatments like this as a cure? The majority of people with Parkinson’s are elderly. How many will be able to stand serious operations? What resources will be required? By referring to a cure we are raising hope in people who will never be eligible for surgery.
I agree that we don’t want to do too much post-hoc analysis but since this trial started there has been an increase in thinking that there may be different types of Parkinson’s. Can we identify from the trial the types of people who are more likely to benefit and concentrate on them.
It would appear that all those who were recruited were passionate about GDNF. Under these circumstances it seems a placebo effect may be more likely. The solution may be how to harness the placebo.
Does this say anything about the value of animal models? Animals don’t get Parkinson’s but they are often used in the testing of new treatments.
LikeLike
Hi Richard,
I hope all is well. Thanks for the thought provoking comment – much appreciated.
We must be very careful with the word ‘cure’. It is emotive and – as you suggest – it raises expectations. It is only recently that I have come to realise that this is one of the great disconnects between “planet patient and planet researcher”. Researchers view ‘cure’ as a problem solving exercise, patients have a lot more at stake.
And yes, surgical procedures are not an ideal path forward, especially if general anesthetics are potentially having a detrimental effect (https://scienceofparkinsons.com/2018/04/07/anesthetics/). In addition, if surgical procedures increase the risk of placebo response (see comments above), it would be better to focus on less invasive, more user friendly approaches like the orally administered compounds companies like Genecode (see post) are developing.
The post hoc analysis should be quick. If there are no obvious characteristics about the responders, it would be wrong to dig too deep into such a limited pool of data. But yes, I agree the investigators should have a look if they haven’t already (and I suspect they have).
As for animal models of PD, they are very poor. Most involve a rapid onset of cell loss (which is probably not disease-relevant) by neurotoxic methods (which is probably not disease relevant), and the experimental treatments are give to those models either just before or just after the cell loss has been initiated (which is definitely not the situation in the clinic). In the case of the GDNF trial, where some participants have had the condition for 10 years+, one can assume that the brain has compensated and adapted over time, which could make a treatment like GDNF redundant (it’s hypothetical possibility at least). In addition, some of the more disease-relevant animals models (such as increasing levels of the Parkinson’s-associated protein alpha synuclein) have suggested that GDNF has no effect (for example: https://www.ncbi.nlm.nih.gov/pubmed/21712347).
And regarding animals not getting Parkinson’s… please see the next SoPD post in a day or so!
Thanks again for the interesting comment.
Kind regards,
Simon
LikeLike
“This trial started with some mighty big expectations on the part of everyone involved (both the participants and the coordinators)…..
We need to have a careful think about managing expectations going forward”
Another thought provoking article! Difficult to manage expectations with the hype ongoing from the excellent BBC2 films..
LikeLike
Hi Keith,
I hope all is well. Yes indeed, we need to be careful with expectations. My greatest concern right now is the large number of folks rushing to be part of the next Exenatide Phase III study because they have read about it having interesting effects on silly websites like the SoPD! I am my own worst enermy. I don’t blame them, but I do worry about expectations and the risk of a placebo response. Perhaps I should remove this website from the web? 🙂
And I have watched the first episode of the BBC documentaries, which I thought was well balanced (I say that from the standpoint of a research I guess). I initially thought the idea of filming a clinical trial utterly dreadful, but it is an interesting insight into both sides of the equation. I would be interested to hear your thoughts on it. Knowing what we know now, I am curious (and apprehensive) about the next episode.
Kind regards,
Simon
LikeLike
Again, thanks and congratulations to Simon for such a comprehensive and accessible account of the science of the GDNF story and its fascinating role in PD. A very useful summary of the field.
As a medical statistician who has been involved with randomized controlled trials in cancer over the last couple of decades, I am impressed with the Bristol team’s undertaking and execution of the GDNF trial. Placebo-controlled trials are challenging at the best of times, notoriously so with surgical treatments. Many surgeons would not wish to undertake such studies, not to mention patients. That is the reason for the Bristol compromise of offering 40 weeks of blinded treatment followed by an open phase of the same length. Judging by the quality of the assembled data, I regard the successful completion of the trial as little short of heroic. And it’s not just because I am a Bristol resident …
Regarding the much-vaunted placebo effect, as far as I understand it in any detail, the motor UPDRS score is partly a PRO (patient-reported outcome) and as such is prone to psychological characteristics of the patients. I can well understand someone on the placebo arm who is “passionate about GDNF” believing that they were on the research treatment and responding accordingly, perhaps even physically – why not? Hope never dies.
One should remember that a statistical comparison between groups of 17 and 18 patients is prone to the vagaries of the observations, and therefore that p-values comparing the groups are distinctly fragile. This is true even in much larger trials, let alone a phase II. As a PwP myself, I find quite encouraging the fact that the larger estimated reduction in UPDRS over baseline in the GDNF arm than in the control arm is maintained at a decent level from week 16 onwards. I would love to see “spaghetti plots” of the individual change profiles in each group. Although inevitably messy, they do often give more insight into the data than summaries of means and SDs at each time point (as in the Whone 2019 paper, Figure 2A). Figure 2B, showing “responders”, is interesting, but as has already been said by other folk, should be very carefully interpreted – suggestive perhaps, but no more than that at this stage. But indeed hopeful.
I do agree with Richard Windle that this surgical approach is likely not a “cure” for PD and may be unattractive or impossible for older folk who are not up to such brain surgery. I still think that the discovery of carbidopa/levodopa treatment in the 1960’s was the most important “breakthrough” in PD management so far achieved, although I do of course understand that the disease continues its inexorable heavy tread nevertheless. Like some types of cancer, finding a cure for such a complex disease as PD is hard. But who knows …
LikeLike
Simon,
Absolutely fantastic review of GDNF, both scientifically and historically. I thought I knew a lot about GDNF and the backstory. Now, I realize how much I didn’t know. We need a group effort now to get a Phase 3 funded, designed and recruited ASAP. I would hate to see another decade go by as we wait. This also makes me think it could be worthwhile to revisit GM-608, which as a small peptide, can cross the BBB if given intravenously.
Great job!!
Best,
Gary
LikeLike
Hi Gary,
I hope all is well. Glad you liked the post – a bit of a beast and completely at odds with my new year’s resolution to write shorter posts, but it was utterly fascinating to revisit some of the older parts of the rollercoaster. Another decade won’t go by (famous last words) before more happens in this area. The CDNF safety results will be announced at the AD/PD meeting at the end of March (full results next year), and the AAV-GDNF trial in the US and EU will kick off in the summer (results 2021/22 perhaps). If I’m honest, I think the prudent thing to do is wait for those results before exploring GDNF any further, but I appreciate that I have the luxury of being able to say that. Others may not be so patient. But the invasiveness of this current approach worries me, and there are so many alternative potential therapies waiting on the sidelines to be evaluated it is difficult to justify further exploring this at the expense of those other approaches (a controversial statement purposefully placed here to elicit a response).
Would love your thoughts on this.
Kind regards,
Simon
PS I still haven’t heard anything from Genervon regarding GM-608. Complete radio silence.
LikeLike
Simon, I’m going to keep posting till you ban me 🙂
Interesting data just published on yesterday GDNF and BDNF in the SN and other regions after ibogain consumption.
https://www.frontiersin.org/articles/10.3389/fphar.2019.00193/full
Growing data there on the anti-addiction efforts. Sounds like they think the GDNF/BDNF boost assists with neuroplasticity for long term benefit.
Think we’ll ever see some PD data? Would be interesting if sub-trip daily consumption would be beneficial and safe.
LikeLike
Thanks for such an incredibly informative article which caters for those of us with little or no scientific background. Plain English. Having been a participant on the recent Bristol trial I have studied this article with interest and have learnt more about the background to GDNF.
I was totally dismayed when the results were published but believe it is not the treatment that didn’t work, just a failure of the trial to prove it. How can you measure that additional energy that I gained, a decrease in that feeling of utter lethargy, a decrease in the duration and frequency of muscle spasms in my feet, the fact that I could walk the length of the exceedingly long corridor in Southmead hospital after two infusions where I previously needed a wheelchair. The UPDRS fails to measure many of the symptoms that I displayed prior to GDNF, whilst placing great emphasis on percentage improvement in symptoms that I have never displayed and therefore have no scope to improve on. It was doomed from the start.
I am sure that when Episode 2 of the BBC2 documentary is shown, it will highlight why the perception of many of the participants is at odds with the official results.
PS Apologies if there are several versions and several copies of this post as my enthusiasm to hit the “post comment” button has over excited my PD symptoms.
LikeLiked by 3 people
Hi Lesley,
Many thanks for your comment – i am pleased that you liked the post. I was at the Florence Pite Memorial evening last year where you presented a truly inspiring lecture (from 6:50 minutes in – https://www.youtube.com/watch?v=qRyNrqSkhlI&t=421s – I hope you don’t mind me sharing the link here). And I also found your recent reflection piece on the Parkinson’s UK Medium webpage equally interesting (https://medium.com/parkinsons-uk/reflections-on-the-gdnf-trial-710bd112b276).
I agree with everything you have said and I would be very interested in learning how (specifically) the process of assessment could be improved. As I suggested in the post, let’s making the GDNF trial the trigger for change – I think everyone involved would be on board with this idea.
Kind regards,
Simon
LikeLike
In the trial (PMID: 17432712) where patients developed antibodies to GDNF – how did that happen? I thought the brain/CNS was a site of immune privilege…
LikeLike
Hi Rhyothemis princeps,
Thanks for the comment. The brain is immune privileged, but immune cells still get in there, particularly in chronic neurodegenerative conditions like Parkinson’s and Alzheimer’s where the blood brain barrier can be compromised. This does not explain why the more recent clinical trial did not detect any antibodies though. It is a mystery that really intrigues me.
Kind regards,
Simon
LikeLike
I wonder if the lack of antibodies in the latest trial could be due to the more advanced surgical techniques employed. Perhaps the surgical trauma of the earlier methods had the effect of providing an inflammatory signal (similar to that of an adjuvant in a vaccine) that caused the immune system to identify the GDNF as foreign and hostile, resulting in the production of antibodies. The more refined technique of the present trial might have resulted in less trauma and thus a smaller chance of antibody production getting triggered.
LikeLike
Thanks so much for this well-written and really interesting discussion re the results, Simon. The whole thing is clearly tantalising. I confess I have wrangled it every which way but loose (well, within my non-trained-neuroscience limits) as I wanted to be responsible in the way we finish the series tomorrow night. End of day, though, and in acknowledgement of the study’s caveats, there would seem to me (with yet more caveats) to be enough here to have another go at it. I very much hope to be filming the sequel.
Jemima
(Director: “The Parkinson’s Drug Trial: A Miracle Cure?”)
LikeLike
Hi, M. Harrison
Could you explain, why it is not possible anymore to watch the 2.part of the documentary ?? (from Switzerland) ??
Thanks in advance,
JANVAN
LikeLike
Hi Simon. Table 2 p 519 of the Brain article, which you posted above (the outcome of the gdnf group W0-W40) shows IMO a bi-modal frequency distribution i.e. there are two groups of gdnf patients, A and B say. One with a big improvement in UPDRS (A) and one very similar to placebo (B) (i.e. gdnf did not add anything). Its a small sample of course but the groups look equally sized with similar sd. So they need to find clinical criteria that distinguishes the two groups of PWPs or else they will never pass the trial stats boxes. There GDNF therapy worked really well for group (A).
LikeLike
Reading your review of the difficult history of this decades-long project helped me to appreciate the commitment and attention span required to bring a project like this to fruition. And despite the failures, it seems that a lot is being learned. As the saying goes: “Try again. Fail again. Fail better.”
I wonder if the lack of antibodies in the latest trial could be due to the more advanced surgical techniques employed. Perhaps the surgical trauma of the earlier methods had the effect of providing an inflammatory signal (similar to that of an adjuvant in a vaccine) that caused the immune system to identify the GDNF as foreign and hostile, resulting in the production of antibodies. The more refined surgical technique of the present trial might have resulted in less trauma and thus a smaller chance of antibody production getting triggered. Just an idea.
Regarding the somewhat paradoxical lack of significant UPDRS change vs. the clearly increased dopaminergic activity, could it be that dopamine *receptors* have atrophied, so that greater dopaminergic activity did not result in greater completed synaptic firings? Perhaps those patients who had a better UPDRS response had better-preserved receptors. DAT scans measure reuptake, right? So I wonder if the dopaminergic axon terminals could be firing and reuptaking the dispensed dopamine, resulting in increased activity being visible on the scans, while at the same time not actually triggering anything on the receiving side of those synapses that had damaged dopamine receptors. Again, just uninformed speculation on my part, but quite interested in your thoughts on whether it might be the cause of the discrepancy.
LikeLike
Hi Simon !
First of all, thank you very much about this extensive artikel, who gives a broad view on the trial.
Is it still possible to watch part 2 of the documentary ??? (In the UK)….because the country where I am
now it is not possible anymore, already after a couple of days,……..
And now…..what will they do ?? First collect money and then continue ‘?? Or will they give up the whole project ??
Greetings !
LikeLike
Here is a link to the two-part BBC series on the GDNF Briston trial, but it only seems to work for those in the UK (which I am not):
https://www.bbc.co.uk/iplayer/episodes/m0002tjw/the-parkinsons-drug-trial-a-miracle-cure
LikeLike
This lecture, at 593 seconds in, points out that because idiopathic PD can be presumed to result from distinct disease processes for different persons, we need to look for improvement in *subsets* of the tested patients whose specific disease processes might susceptible to the specific mode of treatment. So, maybe that is why certain patients had a really good effect, and other had a lesser effect.
We just need to know why some patients responded better than others.
LikeLike
Great article Simon. The failure of the trial seems like such a ridiculous outcome after seeing the phenomenal transformation in some of the participants.
It occurs to me that it may have been better if there had been a washout period between the blinded and open label phases, this could perhaps have shown how long it took each of the groups UPDRS scores to return to baseline – I suspect that the best responders maybe still haven’t.
Also, and without wishing to sound macabre, I find myself wondering if Tom’s brain was examined post-mortem following his tragic and untimely death – surely that would have provided the best evidence as to what was actually happening as a result of the infusions?
Ultimately though I think it just leaves us PwP feeling disappointed and frustrated that once again GDNF shows so much promise and huge improvements in trial participants yet we may never get to benefit from it. I know that CPT have a specific campaign running to raise funds for a further trial and there are some amazingly generous donations coming in, but how much is required and how likely is it that the target will ever be reached? Maybe an 80s style totaliser is in order!
LikeLike
The second episode of the GDNF Bristol trial has just been shown on Norwegian broadcasting, and I was shocked by the conclusion drawn in the end. 42 people made themselves disposable for the medical industry, and when Pfizer finds that its not worth going any further into this study, the trial is just stopped!! What about the pations that normally would decreased in functionality year by year, now suddenly increased significantly, as much as 60%!!!! Should not those people, as a reward for their efforts, get continous treatment so their life quality could get better? And the vage argument of “the company Medgenesis had very little GDNF left at that point”, is in my opinion very thin, as they could easily produced more of it so that could happen, even if both the medisin and the treatment is expensive. And what if long term treatment (not weeks, but years of treatment) actually gave a significant result, what a great victory it would be? I felt very sad when I realized that the participants suddenly where left alone without any more treatment. This is a disgrace for the medical industry. I hope that Gill and his people can continue the project.
LikeLike
Hi, Simon, thank you very much for your last post (about “gluing”).
At the end you referred also a bit to the GDNF-Trial… is there something happen there,
or stands everytihng still ??
LikeLike