At the bottom of our previous post, we mentioned that Japan is the only country where women have a higher incidence of Parkinson’s disease than men.
We also suggested that we have no idea why this difference exists. Well, a study presented at the Cardiovascular, Renal and Metabolic Diseases conference in Annapolis City (Maryland) last week may now be able to explain why this is.
The prevalence of Alzheimer’s disease is significantly higher in women compared to men. One recent estimate suggested that almost two-thirds of individuals diagnosed with Alzheimer’s disease are women (More information here). One possible reason for this is that Alzheimer’s disease is a condition of the elderly and women live longer.
So why is it then is the exact opposite true in Parkinson’s disease???
Source: The Telegraph Newspaper
Men are approximately twice as likely to develop Parkinson’s disease as females (More information here)
In addition, women are on average diagnosed 2 years later than men (More information here)
This gender difference has long puzzled the Parkinson’s research community. But now a group from the University of North Texas Health Science Center think that they may have the answer.
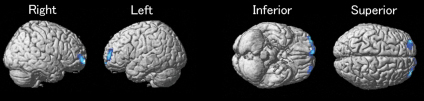
The researchers – lead by Shaletha Holmes from Dr Rebecca Cunningham’s lab – observed that when they stressed dopamine neurons, adding the male hormone testosterone made the damage worse. Interestingly, they found that testosterone was doing this by acting on a protein called cyclooxygenase 2 (or COX2). When they blocked the actions of COX2 while stressing dopamine neurons, they found that they also blocked the damaging effect of testosterone. The researchers concluded that testosterone may exacerbate the damage (and death) in dopamine neurons that occurs in Parkinson’s disease, thus possibly explaining the sex differences described above.
Now, there are several interesting aspects to this finding:
Firstly, the use of Ibuprofen, the nonsteroidal anti-inflammatory drug used for relieving pain, has long been associated with reducing the risk of Parkinson’s disease (More information here).
Ibuprofen is a COX2 inhibitor.
But more importantly, several years ago it was shown that Japanese men have lower levels of testosterone than their Western equivalents. Here is the study:
Title: Evidence for geographical and racial variation in serum sex steroid levels in older men.
Authors: Orwoll ES, Nielson CM, Labrie F, Barrett-Connor E, Cauley JA, Cummings SR, Ensrud K, Karlsson M, Lau E, Leung PC, Lunggren O, Mellström D, Patrick AL, Stefanick ML, Nakamura K, Yoshimura N, Zmuda J, Vandenput L, Ohlsson C; Osteoporotic Fractures in Men (MrOS) Research Group.
Journal: Journal of Clinical Endocrinol. Metab. 2010 Oct;95(10):E151-60.
PMID: 20668046
The study suggested that total testosterone levels (while similar in men from Sweden, Tobago and the US) were 16 per cent higher in men from Hong Kong and Japan. BUT – and here’s the catch – Japanese men also had higher levels of a testosterone-binding hormone (Sex hormone-binding globulin or SHBG), so there is less of the testosterone floating around free to act. As a result, Japanese men had the lowest levels of active testosterone in the study.
Intriguingly, the researchers found that Japanese men who emigrated to the US had similar testosterone levels to men of European descent, suggesting that environmental influences may be having an effect of testosterone levels. Diet perhaps?
If testosterone is found to play a role in the gender difference found in Parkinson’s disease, the lower levels of free testosterone observed in Japanese men may explain why women in Japan have a higher risk of Parkinson’s disease than men.
EDITOR’S NOTE: WHILE WE HAVE NO DOUBTS REGARDING THE RESEARCH OF DR CUNNINGHAM AND HER GROUP, WE ARE TAKING A LEAP IN THIS POST BY APPLYING THE TESTOSTERONE RESULTS TO THE GENDER DIFFERENCE IN JAPAN. THIS IS PURE SPECULATION ON OUR PART. WE HAVE SIMPLY SAT DOWN AND TRIED TO NUT OUT POSSIBLE REASONS AS TO WHY THERE IS A REVERSED GENDER DIFFERENCE FOR PARKINSON’S DISEASE IN JAPAN. OUR THEORY IS YET TO BE TESTED, AND MAY BE COMPLETELY BONKERS. WE PRESENT IT HERE PURELY FOR DISCUSSION SAKE AND WELCOME YOUR THOUGHTS.