|
# # # # Obstructive sleep apnea is a common condition that involves periods of pausing in breathing while one is asleep. Recent research indicates that people diagnosed with this condition may be at higher risk of developing Parkinson’s. Curiously, the same research found that early treatment of the condition reduced the risk of going on to develop Parkinson’s. In today’s post, we will discuss what obstructive sleep apnea is, what the new research found, and how this relates to other neurodegenerative conditions. # # # # |
 Source: ifis
Source: ifis
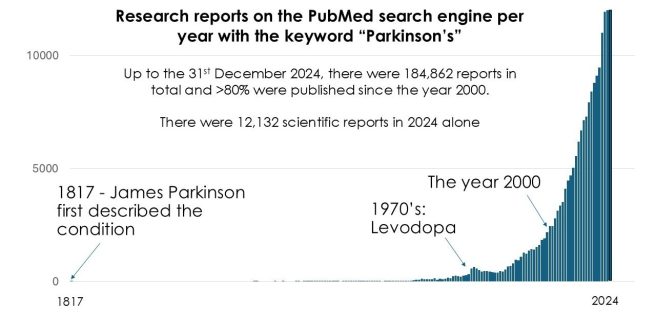
In 2024, there were 12,132 research reports published on Parkinson’s (based on a Pubmed search for the keyword “Parkinson’s”).
That is approximately 33 papers per day.
I think we can agree that that is a lot.
Now, within all of those papers, there are topics that get more attention than others. For example, if you search for the key words “Parkinson’s” and “alpha synuclein” (a hot topic in Parkinson’s) in the scientific search engine ‘Pubmed‘, you will find that there were a total of 13,310 papers from 1997 till 2024. In 2024 alone, there were 1,477 papers published (that’s 4 papers every day!).
Then there are topics that don’t get much attention.
Like “Parkinson’s” and “sleep apnea”.
There were only 32 papers papers published in 2024 (less than three per month).
Ok. But what is sleep apnea?
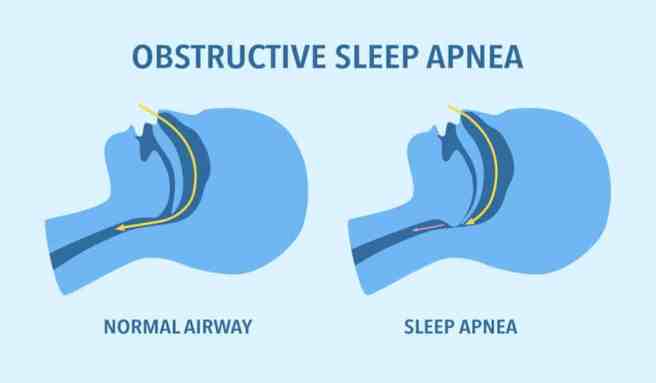
Sleep apnea is a condition when your breathing stops and starts while you sleep. The word “Apnea” comes from the Greek, a- meaning ‘without’ and pnein meaning ‘to breathe’.
The most common type sleep apnea is called obstructive sleep apnea.
Obstructive sleep apnea occurs when the throat muscles relax and block the airway. This happens off and on many times during sleep.
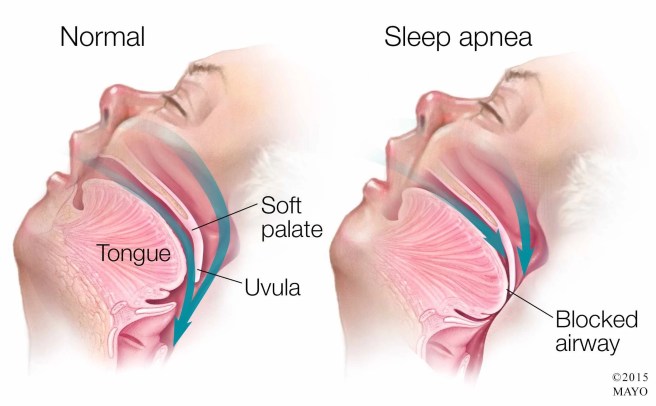 Source: Russellandbodedentistry
Source: Russellandbodedentistry
The symptoms of obstructive sleep apnea during the night include:
- Loud snoring.
- Pauses in breathing during sleep.
- Waking during the night gasping or choking.
- Needing to urinate often.
Symptoms of obstructive sleep apnea during the day include:
- Excessive daytime sleepiness.
- Waking in the morning with a dry mouth or sore throat.
- Morning headaches.
- Trouble focusing.
- Mood changes, such as feeling depressed or being easily upset.
- High blood pressure.
I snore… a lot. And I always feel tired. I am wondering if I have this. Is it common?
Yes, it is common. In fact the American Medical Association believe that an estimated 30 million people in the U.S. might be affected, but only 6 million have been diagnosed with sleep apnea.
How is it measured?
The severity of obstructive sleep apnea is determined by how many breathing pauses you have per hour of sleep. These episodes are measured using the apnea-hypopnea index (AHI).
Severity is measured using the following criteria:
- mild – an AHI reading of 5 to 14 episodes an hour
- moderate – an AHI reading of 15 to 30 episodes an hour
- severe – an AHI reading of more than 30 episodes an hour (Source)
And how is it treated?
Treatment options for obstructive sleep apnea include lifestyle changes (weight loss, side sleeping, cessation of smoking, and avoiding alcohol/sedatives) as well as oral appliances that provide Continuous Positive Airway Pressure (CPAP) therapy. A CPAP machine pumps air into a mask that you wear over your mouth or nose while you sleep.
 Source: rxivpharmacy
Source: rxivpharmacy
Ok, but what does obstructive sleep apnea have to do with Parkinson’s?
Well, obstructive sleep apnea is quite common in Parkinson’s.
A meta analysis was published in 2023:
 Title: Prevalence and clinical aspects of obstructive sleep apnea in Parkinson disease: A meta-analysis.
Title: Prevalence and clinical aspects of obstructive sleep apnea in Parkinson disease: A meta-analysis.
Authors: Maggi G, Giacobbe C, Iannotta F, Santangelo G, Vitale C.
Journal: Eur J Neurol. 2024 Feb;31(2):e16109.
PMID: 37922498 (This report is OPEN ACCESS if you would like to read it)
In this study, the investigators pooled datasets of studies investigating obstructive sleep apnea in people with Parkinson’s and they found that the prevalence was 45% of a total sample of 1448 Parkinson’s patients. They also reported that obstructive sleep apnea in people with Parkinson’s was associated with:
- Older age
- Being male
- Higher body mass index (BMI)
- More severe motor disturbances and periodic limb movements
- Reduced risk of rapid eye movement sleep behavior disorder
- Intake of dopamine agonists
- Worse excessive daytime sleepiness
Curiously no relationship emerged with cognitive functioning and neuropsychiatric features.
Is 45% high?
The investigators suggested that in “the overall prevalence of obstructive sleep apnea in the general population ranges from 9% to 38%“, so yes, 45% is rather high.
Is obstructive sleep apnea associated with a higher risk of developing Parkinson’s?
Yes, and this is where some very recent research is interesting.
Recently this is the report was published:
 Title: Obstructive Sleep Apnea, Positive Airway Pressure, and Implications of Early Treatment in Parkinson Disease.
Title: Obstructive Sleep Apnea, Positive Airway Pressure, and Implications of Early Treatment in Parkinson Disease.
Authors: Neilson LE, Montaño I, May JL, Sicard S, Cho Y, Iliff JJ, Elliott JE, Lim MM, Scott GD.
Journal: JAMA Neurol. 2025 Nov 24:e254691. Online ahead of print.
PMID: 41284280
In this study, the investigators used the electronic health records of 11 310 411 US military veterans (1.1M female veterans [9.8%]) to examine any associations between obstructive sleep apnea and Parkinson’s. Within their dataset, they found 1 552 505 individuals (13.7%) who had been diagnosed with obstructive sleep apnea.
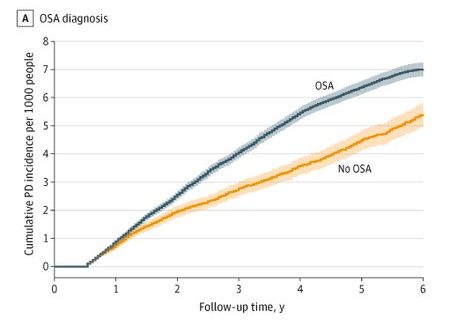
Next they looked at the number of people with Parkinson’s in their dataset and found that veterans with obstructive sleep apnea had 1.61 additional cases of Parkinson’s at 6 years from diagnosis per 1000 people compared to those who had not been diagnosed with obstructive sleep apnea.
What does this mean?
It means that the people with obstructive sleep apnea in the dataset had a higher incidence of Parkinson’s (compared to those individuals without obstructive sleep apnea). You can see it in this graph below, where the blue line (people diagnosed with obstructive sleep apnea) goes up higher over time than the yellow line (people without obstructive sleep apnea). These lines indicate that after a diagnosis of obstructive sleep apnea there is a higher risk of developing Parkinson’s over the years of follow up:
 Source: Twitter
Source: Twitter
Does it depend on the severity of one’s obstructive sleep apnea?
Good question.
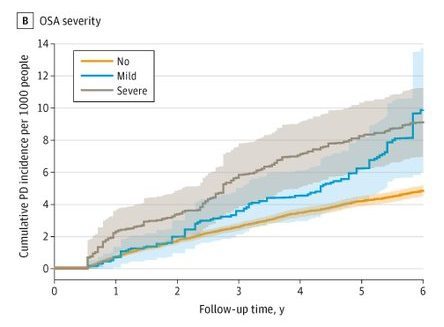
And this is something that the researchers looked into. They explored the data for indications of mild or severe obstructive sleep apnea and this reduced the sample size to 20 905 and 34 607 individuals with mild and severe obstructive sleep apnea, respectively. And when they looked at the incidence of Parkinson’s cases (per 1000 people), they found that severe obstructive sleep apnea was always associated with a higher number of Parkinson’s cases (see the grey line in the graph below and compare it with the blue (or mild severity cases) and the yellow line (no diagnosis)):
 Source: Twitter
Source: Twitter
So mild obstructive sleep apnea has a reduced risk of developing Parkinson’s?
That is what the data suggests in the first few years post diagnosis with obstructive sleep apnea, but as you can see in the graph above the blue line (mild severity) does start to creep up in the later years of the follow up (look at the overlap between the grey and blue lines at 5-6 years post obstructive sleep apnea diagnosis).
Does treatment for obstructive sleep apnea change the risk of Parkinson’s?
Great question!
And this is where the story starts to get really interesting.
How so?
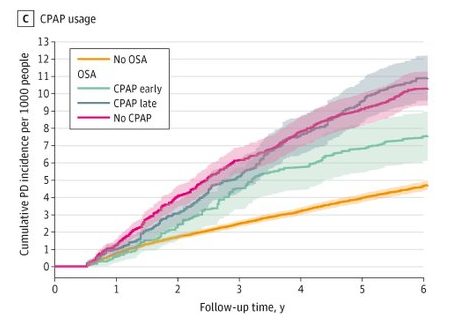
Well, the researchers took their total dataset and asked if initiating CPAP treatment within two years of initial obstructive sleep apnea diagnosis could impact the risk of later development of Parkinson’s.
And what did they find?
They found that there was a significant reduction in incident Parkinson’s as early as two
years after obstructive sleep apnea diagnosis in individuals who received CPAP therapy (compared to those who did not). In fact at 5 years post obstructive sleep apnea diagnosis, there were 2.28 fewer cases of Parkinson’s (per 1000 people) in the CPAP treated group than the no treatment group (at 5 years, the OSA-no CPAP treatment group had 9.10 cases of PD per 1000 people, while the OSA-CPAP treatment group had only 6.81 cases of PD per 1000 people). See the graph below for a visual representation of these trends:
 Source: Twitter
Source: Twitter
Wow. That’s really interesting.
It is. But note in the graph that late initiation of CPAP therapy had no impact on reducing the risk.
Has a reduction in risk of Parkinson’s like this ever been reported before for people with obstructive sleep apnea?
Not for CPAP treatment (not that I am aware of at least – happy to be corrected on this). But other researchers have reported that uvulopalatopharyngoplasty is associated with a reduced risk of Parkinson’s.
Uvulo-what?!?!?
Uvulopalatopharyngoplasty.
Say that three times really fast.
Let me help you: Uvu – lopa – lato – pha – ryngo – plasty.
What is it?
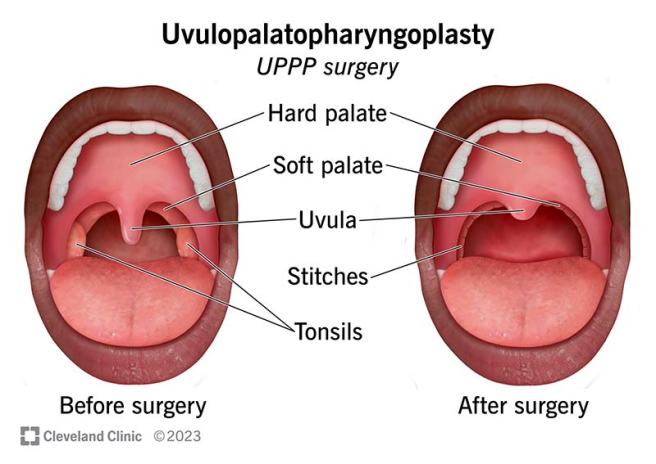
Uvulopalatopharyngoplasty is a common surgical procedure that involves removing excess tissue from the back of the throat (uvula, soft palate, tonsils) to widen the airway. It is primarily employed for treating obstructive sleep apnea and severe snoring when other treatments have failed.
 Source: Clevelandclinic
Source: Clevelandclinic
And this Uvu-lopa-whatever procedure reduced risk of Parkinson’s?
Well, that is what this report published in 2021 suggested:
Title: Uvulopalatopharyngoplasty may decrease the incidence of Parkinson’s disease associated with obstructive sleep apnea.
Authors: Lee HM, Han KD, Suh JD, Cho JH.
Journal: Sci Rep. 2021 May 5;11(1):9608.
PMID: 33953319 (This report is OPEN ACCESS if you would like to read it)
In this study, the investigators collected medical data from the Korea National Health Insurance Service. They screened for people newly diagnosed with obstructive sleep apnea between 2007 and 2014, and they found 202,726 cases. These individuals were then divided into two groups:
- Those who underwent uvulopalatopharyngoplasty (n = 22,742)
- Those who did not (n = 179,984)
A control group (n = 1,013,630) was also selected for comparison sake.
When they looked at the incidence of Parkinson’s over time across these groups, this is what they saw:
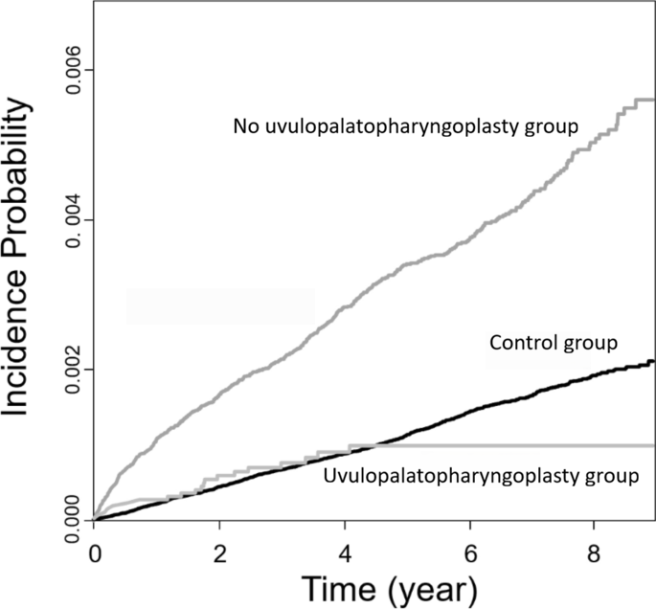 Source: Nature (labels adapted)
Source: Nature (labels adapted)
The uvulopalatopharyngoplasty treated group had the same incidence of Parkinson’s as the control group, while the obstructive sleep apnea group had a much higher incidence. The ‘flat line’ in the uvulopalatopharyngoplasty treated group data from around 4 years was due to the short follow-up period of these patients, which the investigators admitted was a limitation in the study.
So obstructive sleep apnea increases risk of Parkinson’s and early treatment of obstructive sleep apnea reduces that risk?
Exactly.
How?
That’s the million dollar question, isn’t it.
But very recently some researchers have been having a look at possible mechanisms. And they have published their findings in this report:
 Title: Obstructive sleep apnea, biomarker profiles, and clinical progression in Parkinson’s disease: Longitudinal effects of CPAP therapy.
Title: Obstructive sleep apnea, biomarker profiles, and clinical progression in Parkinson’s disease: Longitudinal effects of CPAP therapy.
Authors: Zhu S, An D, Liu X.
Journal: Sleep Med. 2026 Jan 5;139:108766.
PMID: 41499940
In this study, the investigators had a cohort of 140 patients with Parkinson’s, and they found that 72 (51.4 %) of them had obstructive sleep apnea. They collected clinical evaluation data as well as biosamples (blood and cerebrospinal fluid) from everyone in their cohort to explore differences between these two groups.
The researchers found that the individuals in their Parkinson’s + obstructive sleep apnea group displayed higher levels of inflammatory (IL-1β, IL-6, & TNF-α), glial (CHI3L1, GFAP, S100B), and neurodegeneration markers (NfL) than the other group.
Interestingly, among the 72 individuals with obstructive sleep apnea, 58 of them had initiating CPAP therapy, and 29 of these were adhering to the treatment. This adherence was associated with a reduction in apnea-hypopnea index (AHI) scores, but also improvement in Parkinson’s motor score (UPDRS III -0.62 vs + 2.41/year; P < 0.001). There was also lower levels of inflammatory markers in the CPAP treated group.
Has anyone else ever reported an improvement like this from CPAP treatment?
Yes. A clinical trial was conducted recently and the results were published in this study:
 Title: Cognition and obstructive sleep apnea in Parkinson’s disease: randomized controlled trial of positive airway pressure.
Title: Cognition and obstructive sleep apnea in Parkinson’s disease: randomized controlled trial of positive airway pressure.
Authors: Lajoie AC, Lafontaine AL, Kimoff RJ, Benedetti A, Robinson AR, Létourneau M, Crane J, Scanga A, Noel F, Kaminska M.
Journal: Sleep. 2025 Jul 11;48(7):zsaf038.
PMID: 39945727 (This report is OPEN ACCESS if you would like to read it)
In this study, the investigators recruited 94 participants with Parkinson’s and obstructive sleep apnea and they assigned them to either CPAP therapy or nasal dilator strips (this was considered the placebo condition in this study) for a 6-month treatment period. The groups were assessed at 3 months and 6 months using a variety of measures, but the Montreal Cognitive Assessment (MoCA) was used as the primary outcome measure:
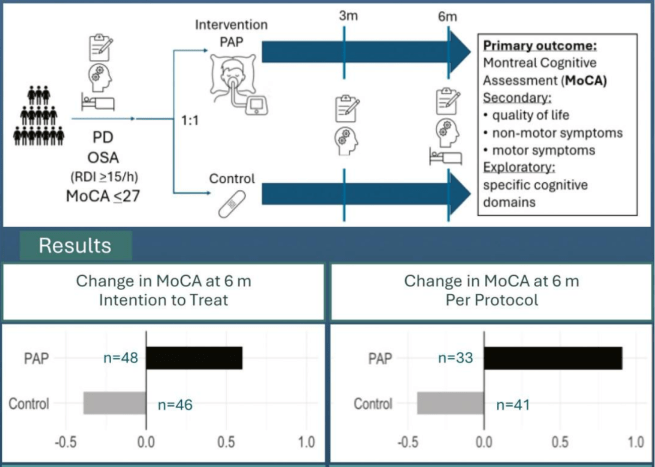 Source: PMC
Source: PMC
At the end of their study, the researchers found that the CPAP group improved on their scores on the MoCA test by 0.60, while the control group’s MoCA scores declined by −0.39. They also reported significant improvements in motor function (as measured by the Movement Disorder Society Revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) part III score) in the CPAP group compared to control group. In nonmotor symptoms, depression measures and sleep quality scores also improved with CPAP.
So there is some data supporting the idea that CPAP may help with Parkinson’s.
Interesting. So, summing up, what does it all mean?
Not just yet. There is still one other detail about sleep apnea that needs to be discussed.
Which is?
Sex.
You have my full attention.
As in gender. It appears that the impact obstructive sleep apnea has on Parkinson’s is stronger in females.
In the Neilson et al (2025) paper reviewed above, the investigators found that all of their findings were stronger in females than males. Females with obstructive sleep apnea in their dataset were almost twice as at risk of Parkinson’s compared to the males.
And this report from 2015 found a similar result:
 Title: A 5-Year Follow-up Study on the Relationship between Obstructive Sleep Apnea and Parkinson Disease.
Title: A 5-Year Follow-up Study on the Relationship between Obstructive Sleep Apnea and Parkinson Disease.
Authors: Sheu JJ, Lee HC, Lin HC, Kao LT, Chung SD.
Journal: J Clin Sleep Med. 2015 Dec 15;11(12):1403-8.
PMID: 26156952 (This report is OPEN ACCESS if you would like to read it)
Using data from the Taiwan Longitudinal Health Insurance Database, the researchers in this study identified 1,532 individuals with obstructive sleep apnea and randomly selected 7,660 people as a comparison cohort. They found that during the 5 year follow up period, the individuals with obstructive sleep apnea were almost twice as likely to develop Parkinson’s as the non-sleep apnea group. And most of this effect was based on the females in the dataset. Females with obstructive sleep apnea were found to be at a significant risk of subsequent Parkinson’s diagnosis during the 5-year follow-up period, while men were not.
This gender effect will require more investigation, but it may be specific to Parkinson’s.
What does that mean?
Well, the risks associated with obstructive sleep apnea are not specific to Parkinson’s. Having obstructive sleep apnea puts one at risk of developing other conditions. And chief among these is dementia.
Obstructive sleep apnea increases risk of dementia?
Yes.
There have been many reports suggesting that obstructive sleep apnea increases risk of dementia, and it represents a modifiable risk factor (Click here and here to read reports on this).
And this risk appears to be higher in males rather than females.
This report was published in 2021:
 Title: Cognitive Function in a Sleep Clinic Cohort of Patients with Obstructive Sleep Apnea.
Title: Cognitive Function in a Sleep Clinic Cohort of Patients with Obstructive Sleep Apnea.
Authors: Beaudin AE, Raneri JK, Ayas NT, Skomro RP, Fox N, Hirsch Allen AJM, Bowen MW, Nocon A, Lynch EJ, Wang M, Smith EE, Hanly PJ.
Journal: Ann Am Thorac Soc. 2021 May;18(5):865-875.
PMID: 33147067 (This report is OPEN ACCESS if you would like to read it)
In this study, the investigators recruited 1,084 individuals who had been referred to three academic sleep centers for suspected obstructive sleep apnea. They conducted sleep and cognitive assessments on these people. The researchers found that cognitive impairment was highly prevalent in individuals referred to sleep clinics for suspected obstructive sleep apnea, particularly in older males with moderate to severe obstructive sleep apnea and concurrent vascular comorbidities.
So while women with obstructive sleep apnea may be at more risk of Parkinson’s, men with obstructive sleep apnea appear to be at higher risk of dementia.
So what does it all mean?
I think my late uncle had obstructive sleep apnea. I suspect this because my Aunt once said “one night I woke up and your uncle was sleeping beside me, but he had stopped breathing”.
Then she added “I wasn’t sure if I should wake him up to tell him. I was worried that he would be annoyed“.
The earnestness with which my aunt shared this information slightly concerned me. But if my uncle did have obstructive sleep apnea, it speaks to how common the condition is. If he did indeed have obstructive sleep apnea, it is important to note that he was of sound mind and body. The risk associations discussed in this post are low – just because someone has obstructive sleep apnea it does not mean that they will definitely go on to develop Parkinson’s or cognitive issues. Sleep apnea simply increases their risk of developing one of these conditions.
What is interesting in the newly published data is that early CPAP therapy and uvulopalatopharyngoplasty reduce the risk of Parkinson’s in individuals diagnosed with obstructive sleep apnea. In the search for risk modifiers, this could be a great example to further explore and implement guidance/recommendations. It could have very real impact.
An Eric Ambler quote has been used as the title of this post, but I don’t think that reality needs to be obstructive to further research in this area. It would be interesting to see how many people in the Michael J Fox Foundation’s PPMI dataset may have obstructive sleep apnea and what impact this has on the progression of their Parkinson’s symptoms. It could also be interesting to test the impact of CPAP therapy on those with Parkinson’s and obstructive sleep apnea – does it reduce the potential for future cognitive complications? I like the fact that enrollment into such a study would be specific to individuals diagnosed with obstructive sleep apnea and the severity of that condition could be included in the participant stratification in any clinical trial.
Not much obstructing this future research. Lots of opportunity and potential.
 All of the material on this website is licensed under a
All of the material on this website is licensed under a
Creative Commons Attribution 4.0 International License
You can do whatever you like with it!
EDITOR S NOTE: The author of this post is an employee of Cure Parkinson s, so he might be a little bit biased in his views on research and clinical trials supported by the trust. That said, the trust has not requested the production of this post, and the author is sharing it simply because it may be of interest to the Parkinson s community.
The information provided by the SoPD website is for information and educational purposes only. Under no circumstances should it ever be considered medical or actionable advice. It is provided by research scientists, not medical practitioners. Any actions taken based on what has been read on the website are the sole responsibility of the reader. Any actions being contemplated by readers should firstly be discussed with a qualified healthcare professional who is aware of your medical history. While some of the information discussed in this post may cause concern, please speak with your medical physician before attempting any change in an existing treatment regime.
The banner for today’s post was sourced from Ladentist
Potentially due to chronic intermittent hypoxia? https://pmc.ncbi.nlm.nih.gov/articles/PMC12712921/
As opposed to acute intermittent hypoxia which might be neuroprotective? https://onlinelibrary.wiley.com/doi/full/10.1002/glia.70127
LikeLiked by 1 person
Thanks Antoine, so do you think that there is something else that differentiates PD from AD, and obstructive sleep apnea is simply an “unmasking” factor?
LikeLike
I don’t understand your question. (btw, sleep apnea was not listed in the 2024 report of the Lancet Commission on dementia as a risk factor due to “insufficient evidence”)
LikeLike