|
Over night new research has been published in the prestigious journal Science. It involves an asthma drug and the results may have MAJOR implications for Parkinson’s disease. Researchers have found that compounds in certain drugs used in the treatment of Asthma, may also have beneficial effects in Parkinson’s disease. In today’s post, we will discuss what those compounds are, how they function, and why this result could be very exciting for the Parkinson’s disease community. |
Norway. Source: Go-today
Another week goes by and yet any potential break-through in world of Parkinson’s disease research.
The pace of the discoveries are coming thick and fast at the moment, and I’ll be honest: I’m having a very hard time keeping up. It’s bonkers! I have so many posts in draft form at the moment, and just when I think I might get one finished there is a new research report being published that demands a post of its own.
Which brings me to the study I’d like to discuss today. And this one is being prioritised with regards to its place in list of pending posts. A large group of researchers from the USA and Norway have just published the results of a project that – I think you’ll agree – are very interesting:
 Title: β2-Adrenoreceptor is a regulator of the α-synuclein gene driving risk of Parkinson’s disease
Title: β2-Adrenoreceptor is a regulator of the α-synuclein gene driving risk of Parkinson’s disease
Authors: Mittal S, Bjørnevik K, Im DS, Flierl A, Dong X, Locascio JJ, Abo KM, Long E, Jin M, Xu B, Xiang YK, Rochet JC, Engeland A, Rizzu P, Heutink P, Bartels T, Selkoe DJ, Caldarone BJ, Glicksman MA, Khurana V, Schüle B, Park DS, Riise T, Scherzer CR.
Journal: Science. 2017 Sep 1;357(6354):891-898.
PMID: 28860381
The researchers who conducted this study began by conducting a massive screening experiment. They wanted to identify drugs that could reduce the production of a protein called Alpha Synuclein (regular readers will be aware that that protein is intimately associated with Parkinson’s disease). So the investigators grew cells that stably produce the human version of Alpha Synuclein and they screened 1126 compounds (including drugs approved by the U.S. Food and Drug Administration (or FDA) as well as wide range of natural products, vitamins, health supplements, and alkaloids.
From this screen they identified 35 compounds that lowered Alpha Synuclein levels by more than 35%. Amongst these 35 compounds was the selective Beta2-Adrenoreceptor agonist metaproterenol. Because metaproterenol is not brain penetrant – meaning that it can not pass through the protective blood-brain-barrier membrane surrounding the brain – the investigators added six related drugs, including the two selective Beta2-Adrenoreceptor agonists, clenbuterol and salbutamol (which are both brain penetrant).
Hang on a second, what are Beta2-Adrenoreceptor agonist?
As I mentioned in the previous post, an agonist is a drug that binds to and activates a particular receptor.
On the surface of a cell, there are lots of receptors which act as switches for certain biological processes to be initiated. Receptors will wait for a protein to come along and activate them or alternatively block them. The activators are called agonists, while the blockers are antagonists.

Agonist vs antagonist. Source: Psychonautwiki
Beta2-Adrenoreceptor agonist are drugs that bind to and activate the Beta2-Adrenergic receptor. These receptors sit in the wall of cells (the membrane), with part of themselves exposed to the world outside the cells (the extracellular space) and another region of themselves exposed to the interior of the cell (the intracellular space).
The Beta2-Adrenergic receptor. Source: Wikipedia
Beta2-Adrenergic receptor interacts with a chemical called epinephrine, which is a neurotransmitter like dopamine. Epinephrine will come floating along, bind to the Beta2-Adrenergic receptor, and activate it. Thus, Beta2-Adrenoreceptor agonists are effectively epinephrine.
And what medical conditions are treated with Beta2-Adrenoreceptor agonists?
They are primarily used to treat pulmonary disorders – that is conditions of the lungs such as Asthma (a common long-term inflammatory condition of the lungs) and Chronic obstructive pulmonary disease (or COPD, which is a progressive obstructive lung disease).
Beta2-Adrenoreceptor agonists cause smooth muscle fibres to relax.
Ok, so these researchers found Beta2-Adrenoreceptor agonists reduce the production of Alpha Synuclein in their screening experiment?
Yes, exactly. The cells treated with Beta2-Adrenoreceptor agonists generated less of the Parkinson’s disease associated protein.
One other interesting compound that the screen also highlighted was a drug called Riluzole. This is an FDA-approved drug for modification of amyotrophic lateral sclerosis (ALS), but it has also been shown to reduce dopaminergic neurodegeneration and provide neuroprotection in a rat model of Parkinson’s disease (Click here to read more).
The researchers next injected some mice with Beta2-Adrenoreceptor agonists and then looked at the dopamine neurons in the brain, and they found that those cells also produced less Alpha Synuclein. Interestingly, they also noted that in mice that did not have any Beta2-Adrenergic receptor, the levels of Alpha Synuclein in the brain were twice as high as normal.
Interesting. But is this relevant to humans?
Well, having established that Beta2-Adrenergic receptor activation reduces Alpha Synuclein levels, the researchers next turned their attention to what is happening in people that have been treated with Beta2-Adrenoreceptor agonists. To do this, the researchers used the Norwegian Prescription Database which contains the complete records of all prescribed drugs dispensed at pharmacies to every individual in Norway since 2004.
They decided to look for prescriptions of the Beta2-Adrenoreceptor agonist, Salbutamol to see whether use of this drug could reduce the risk of developing Parkinson’s disease. Amazingly, they found that Salbutamol was associated with decreased risk of developing Parkinson’s disease – literally a 1/3 reduction in risk.
But (and it’s a BIG ‘but’), the researchers also asked the reverse question: does blocking Beta2-Adrenergic receptor (with an antagonist drug) increase one’s risk of developing Parkinson’s disease?
And guess what they found?
Propranolol is often called a ‘beta-blocker’ because it blocks the Beta2-Adrenergic receptor. This Beta2-Adrenoreceptor antagonist is commonly used to treat high blood pressure and essential tremor. In their analysis, the researchers found that Propranolol was associated with a two-fold increase in the risk of developing Parkinson’s disease! 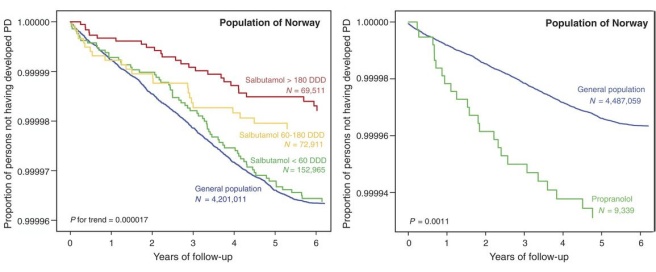
Source: Science
As you can see from the image above, those individuals who took a high defined daily doses (DDD) of Salbutamol (the red line on the left graph) had a lower risk of developing Parkinson’s disease than those who were administered low levels of Salbutamol (the green line – which does not differ from the general population level of risk (blue line)). And on the graph on the right the 9,339 individuals treated with Propranolol (green line) had a higher risk of developing Parkinson’s disease than the general population.
I am currently taking Propranolol! Should I stop?
While I usually do not like to give advice on this website, if you are concerned about this finding it may be wise to ask your doctor whether there are any alternative medications available (especially if you have a family history of Parkinson’s disease).
And although it is a rather staggering result, I will be very interested to see if the same trends are observed in the other big Scandinavian medical databases maintained in Denmark and Sweden. Until the finding is replicated independently we shall wait and see.
Wow. This is interesting. What did the researchers do next?
Next the researchers investigated whether Beta2-Adrenoreceptor agonist (Clenbuterol) treatment could rescue two different mouse models of Parkinson’s disease, and they observed significant levels of neuroprotection of the dopamine neurons in mice after Clenbuterol treatment.
And finally the researchers tested Beta2-Adrenoreceptor agonists on human dopamine neurons in cell culture. The dopamine neurons were generated from human IPS cells (which are stem cells derived from skin cells – Click here to read more about this). The IPS cells were collected from people with a particular type of Parkinson’s disease, which results from having too many copies of the Alpha Synuclein gene (three copies!). These individuals have increased risk of developing Parkinson’s disease. The researchers found that Beta2-Adrenoreceptor agonist (Clenbuterol) treatment resulted in lower levels of Alpha Synuclein in these cells and it also improved mitochondrial function and survival in these cells.
The researchers completed the study by concluding that Beta2-Adrenergic receptor activation reduces levels of Alpha Synuclein and the risk of Parkinson’s disease “and constitutes a potential target for therapies”.
Very interesting! Have Beta2-Adrenoreceptor agonists ever been tested in the clinic before?
That’s the good news: Yes, they have:
Title: “Wearing-off” and beta 2-adrenoceptor agonist in Parkinson’s disease.
Authors: Hishida R, Kurahashi K, Narita S, Baba T, Matsunaga M.
Journal: Lancet. 1992 Apr 4;339(8797):870.
PMID: 1347877
In this study, the Japanese investigators recruited 9 subjects with Parkinson’s disease and gave them the Beta2-Adrenoreceptor agonist Salbutamol (6 mg daily) for two weeks. They found that co-administration of salbutamol with Levodopa significantly increased the mean daily total ‘on’ phase (from 8.3 hours to 9.8 hours – ‘on’ phase being the period of normalised movement). But the researchers did raise one concern: the agonist “can sometimes induce or aggravate postural tremor in Parkinsonism – indeed one patient in our study complained of postural tremor after salbutamol“.
Despite this positive result, the researchers never followed up the study (as far as I can tell). But that didn’t matter, because others were also testing salbutamol in people with Parkinson’s disease as well:
Title: Beta 2-adrenergic agonist as adjunct therapy to levodopa in Parkinson’s disease.
Authors: Alexander GM, Schwartzman RJ, Nukes TA, Grothusen JR, Hooker MD.
Journal: Neurology. 1994 Aug;44(8):1511-3.
PMID: 8058159
In this study conducted in Philadelphia, the researchers administered Salbutamol to 6 people with Parkinson’s disease for 5 days. Five of those subjects demonstrated some improvements in particular movement tasks (such as a 30% increase in finger tapping), but there was little or no change in the levels of rigidity or the severity of resting tremors. Curiously, the improvements were also maintained over time with continued Salbutamol treatment (2mg x 3 per day).
A third group of researcher found that Beta2-Adrenergic receptor activation helps with Levodopa treatment in animal:
Title: beta-Adrenergics enhance brain extraction of levodopa.
Authors: Uc EY, Dienel GA, Cruz NF, Harik SI.
Journal: Mov Disord. 2002 Jan;17(1):54-9.
PMID: 11835439
This study suggested that Beta2-Adrenoreceptor agonists might be useful in the treatment of Parkinson’s disease because it enhances the delivery of Levodopa to the brain. This effect appears to be peripheral to the brain as both brain penetrant and non penetrant Beta2-Adrenoreceptor agonists provided this benefit.
Given this interesting result in animals, the researchers next wanted to look at what happens in humans, which resulted in this research report:
Title: Albuterol improves response to levodopa and increases skeletal muscle mass in patients with fluctuating Parkinson disease.
Authors: Uc EY, Lambert CP, Harik SI, Rodnitzky RL, Evans WJ.
Journal: Clin Neuropharmacol. 2003 Jul-Aug;26(4):207-12.
PMID: 12897642
In this open-label study, 8 people with Parkinson’s disease but not experiencing dyskinesias underwent 14 weeks of treatment with Albuterol (aka Salbutamol – 4 mg x 4 per day). After this treatment, UPDRS motor scores improved by 9.8% and finger tapping improved by 7.6%. Four of the participants had a mild global improvement, and 3 of them chose to continue Albuterol beyond the termination of the study. Of note, however, is that the mean heart rate of all the participant increased from 78.3 beats/minute to 85.6 beats/minute, which is a known side effect of Beta2-Adrenoreceptor agonist treatment.
Are there any other side effects to Beta2-Adrenoreceptor agonist treatment?
Tachycardia – which is a heart rate that exceeds normal levels – is the main side effect of this class of drugs. Thus anyone with a history of heart issues should be weary of considering these drugs. There have also been reports of excessive sweating, anxiety, insomnia, agitation and (I kid you not) tremor.
So what does it all mean?
In the wake of the recent Exenatide results, it would be very easy to get overly excited as we are suddenly confronted with another clinically available drug that may have beneficial effects on Parkinson’s disease. But while it appears that Exenatide is doing something in Parkinson’s disease based on the 60 person phase II clinical trial results that were recently released (Click here for more on this), it is not clear that Beta2-Adrenoreceptor agonist are having an impact on the condition.
What we have here is an interesting biological effect (reduced levels of a Parkinson’s-associated protein, Alpha Synuclein), a very curious correlation in Norway, and a series neuroprotective studies suggesting that this class of drugs is worthy of further investigations. The small clinical studies that I mentioned above are exactly that: small. Too small in fact to conclude very much (other than Beta2-Adrenoreceptor agonist appear to be safe in PD subjects). All of these results need to be independently replicated before proper conclusions can be made.
Thus, readers should not be rushing to their doctors and demanding for an asthma inhaler.
Dr Clemens Scherzer – one of the researcher who conduced the new study – suggests that it would be wise to try to refine the Beta2-Adrenoreceptor agonist compounds, to make them more effective at reducing levels of Alpha Synuclein. This process would also give us an opportunity to further research this potential therapeutic pathway. Such a refined drug could then be taken to the clinic and perhaps be firstly tested on people with Parkinson’s disease that involve genetic triplication of the Alpha Synuclein gene.
EDITORIAL NOTE: The information provided by the SoPD website is for information and educational purposes only. Under no circumstances should it ever be considered medical or actionable advice. It is provided by research scientists, not medical practitioners. Any actions taken – based on what has been read on the website – are the sole responsibility of the reader. Any actions being contemplated by readers should firstly be discussed with a qualified healthcare professional who is aware of your medical history. Please speak with your medical physician before attempting any change in an existing treatment regime.
The banner for today’s post was sourced from Bookmartialarts





Thanks. Sounds really hopeful.
LikeLike
Indeed Dkdc. Glad you liked it.
LikeLike
Simon. Thank you so much for the prompt post! This news is 48 hours old or so? And we get the rundown from you on a Saturday no less. Great!
It seems to me like as in most great mistakes or catastrophes, that upon looking back after the fact it becomes clear that tradgey could have been averted at several points in time by several factors. So with us with PD it seems that we’ll find eventually that there are several factors overlapping that put us in just the right “unlucky equilibrium” that has put us here. As we walk along the perfect little knifes edge that puts us in the neudegeration zone, research keeps finding more little clues pointing us where and how to nudge the system back to normal operation.
On days like this it sems that we’re getting closer to asking “when” and looking back at “if”.
Great motivation for a trip to the Gym to go rescue neurons. Hold tight everyone. We’re going to beat this together.
LikeLike
Hi Double,
Thanks for your comment – glad you liked the post. Admittedly it was a bit of a rushed job.
I often wonder if my 5 year old daughter will ever learn to drive a car. By that I mean: we are living in a brief period between horses and automated vehicles, during which the powers-that-be reckless allow us to drive ourselves (imagine what future generations will think!). And with the incredible pace of technological development and all the various groups around the world focused on robot cars, the ‘when’ does not feel very far away.
I also wonder if my daughter’s generation will ever have to worry about Parkinson’s disease. 10 years ago major research results were being published once or twice a year, and now it’s literally once or twice per week! It really is hard to keep up, but thankfully the jigsaw puzzle is coming together nicely.
There is no ‘If’, there is only ‘when’.
Simon
LikeLike
I think a key detail is that the authors proposed that the agonists might act via a very specific mechanism, targeting a particular gene promotor. This would be a very useful observation, because (i) it identifies a site for which new drugs can be designed and (ii) it means that Beta-agonists are not working by a general increase in metabolism.
chris
LikeLike
Hi Chris,
Thanks for the comment. It is a really interesting observation.
I have to admit that I sat for a long time trying to work out how to explain in layman’s terms that ‘Clenbuterol treatment reduced H3K27 acetylation across the SNCA promoter’. In the end (and rushed as I was) I figured that it was one detail that my mum (my most avid reader) didn’t need to worry about and so I just gave up and moved on. When I have some spare time I might go back and add a section on what a promoter is and how they are regulated. I would actually like to do this though, because another interesting observation in the results was the increase in SNCA transcripts following Valproate (Valproic acid) treatment (which is used to treat epilepsy, bipolar disorder and migraines – see figure 3). Perhaps the Scandinavian bioinformaticians (Karin Wirdefeldt & co. at the Karolinska) could add this drug to their list to check for associations with PD.
Kind regards,
Simon
LikeLike
Albuterol study of great interest as impacted a-syn, the cause of PD. In 14 weeks, 4/8 participants had mild global improvement, very nice result. The big question, what would be the decreased risk of dementia in 10 years. Since Albuterol is a cheap generic, don’t expect that study. Translation of what researcher said: “If we can make a super expensive brand name knock-off of Albuterol, then we will have potential blockbuster drug worth testing.”
LikeLike