|
# # # # At the end of each year, it is a useful process to take stock and review what we have learnt over the last 12 months. 2022 has been an extremely busy year for Parkinson’s research, with a lot of clinical trial results and new insights. As the world continues to re-open from the COVID-19 pandemic, there has been a continually rising tide of new research results and interesting new developments. In today’s post, we will consider three big Parkinson’s-related research takeaways of 2022 (based on our humble opinions here at the SoPD), and then we will provide an extended overview of some of the important pieces of news from the last 12 months (Be warned: this will be a rather long post). # # # # |
 Knatchbull-Hugesse. Source: Getty
Knatchbull-Hugesse. Source: Getty
Hughe Knatchbull-Hugessen, the British Ambassador to China between 1936-1937 wrote in his memoir that before he left England for China, a friend told him of a Chinese curse, “May you live in interesting times” (Source).
I never really understood why this quote was considered “a curse”. Surely living in boring times would be more tortuous.
But the noise and chaos of recent years have really hammered home the nature of this curse. There were many days this year where I was wishing for less interesting times.
 2022. Source: Wikipedia
2022. Source: Wikipedia
That said, 2022 has been a fascinating experience. The full spectrum of human emotions has been elicited: From the highs of the football world cup to the horrors and catastrophic consequences of Russia’s ignominious invasion of Ukraine.
From the glorious achievements (such as the James Webb space telescope and a net energy gain from a fusion reaction), to the unfathomable idiocies of the UK and US political class (seriously, in the UK we had 3 prime ministers, 4 chancellors, and one gut wrenching “mini budget” disaster that showed the true fragility of our underfunded pension schemes) – 2022 had it all.
There were also an amazing array of new discoveries and insights in Parkinson’s research. And while such a statement may not bring much solace to those living with condition, it is tremendously encouraging to see the furious rate at which these findings are announced.
In this, the last SoPD post of 2022, we will look back and review the last 12 months by providing an overview of those pieces of research news that we here at SoPD HQ thought were most interesting. We apologise to any researchers who do not get a mention here (by all means feel free to berate us in the comments section below if you think we missed something key), but these were the announcements that really grabbed our attention.
|
# EDITOR’S NOTE: The author of this blog is the director of research at the medical research charity Cure Parkinson’s. For the purpose of transparency and to eliminate any sense of bias, where Cure Parkinson’s is a funder of the research it shall be noted. # |
The 3 main SOPD highlights in Parkinson’s-related research for 2022
(in no particular order)
1. The results of the Phase 2b randomized, placebo-controlled, double-blind KARMET study of ENT-01:
In January 2022, the biotech company Enterin announced the results of their Phase 2b randomized, placebo-controlled, double-blind KARMET study of ENT-01 (a derivative of squalamine that the company has been developing). The trial involved 150 individuals with Parkinson’s and constipation. Following a 2-week baseline assessment period, the participants randomized to receive ENT-01 or placebo. A 25-day treatment period was followed by a 2-week phase when all participants were placed on placebo before a 4-week wash-out (Click here to read more details about this study).
The results of the study indicated that ENT-01 is safe & well tolerated. In addition, the primary endpoint of the study (the predetermined measure of success – in this case, the degree of change in complete spontaneous bowel movement from baseline to the end of the 3-week treatment period) was met. The researchers found that bowel movement was significantly better in the treatment group compared to placebo – and this improvement was maintained after the treatment was stopped (at least 6 weeks).
 Source: Enterin
Source: Enterin
While this result was pleasing to see, the truly remarkable finding was slightly deeper in the data: 13 of the participants had suffered from symptoms of psychosis before joining the study. Six of these individuals were randomly assigned to the ENT-01 treatment group, and the researchers observed a reduction in the levels of psychosis (as measured by SAPS-PD) during the 4 week treatment period, and this effect persisted out to 6 weeks post-termination of treatment:
 Source: Enterin
Source: Enterin
This was a really interesting effect because this drug (ENT-01) has very low bioavailability and only acts locally in the gut. So this head scratching outcome in the brain points towards some intriguing interactions within the gut-brain axis. We’re really looking forward to seeing the next steps in the development of ENT-01 (Click here to read more about this story).
2. Initiation of Luminare and Lighthouse
In the next SoPD post (the annual “Road Ahead” report), we will discuss how two decades of research stemming from the discovery of genetic risk factors for Parkinson’s is now paying dividends in the form of clinical trials targeting the biology associated with those variations. One of the best examples of this progress is the “Lighthouse” and “Luminare” clinical trials.
In 2022, Denali Therapeutics and Biogen initiated two large clinical trials evaluating LRRK2 inhibition in Parkinson’s cohorts. “The Lighthouse Study is a global Phase 3 trial expected to enroll approximately 400 Parkinson’s participants with LRRK2 mutations“. The treatment period will be at least 96 weeks for this study (because LRRK2-associated PD is a slow progressing form of PD) and the primary endpoint will be change in MDS-UPDRS from baseline.
“The Luminare Study is a global Phase 2b trial expected to enroll approximately 640 participants with Parkinson’s who do not carry a LRRK2 mutation & is designed to potentially support registration of BIIB122“. The minimum treatment period for the Luminare study will be 48 weeks and like the Lighthouse study the primary endpoint will be change in MDS-UPDRS from baseline.
Both of these studies have come from the discovery that genetic variations in the LRRK2 gene can increase the risk of developing Parkinson’s (discovered in 2004), and the last decade of developing the LRRK2 inhibitor (called BIIB122, formerly known: DNL151) that is being tested in the trials. This agent has previously been shown to reduce levels of LRRK2 activity in people with Parkinson’s (at all doses tested):
 QD means ‘once a day’. Source: Denali
QD means ‘once a day’. Source: Denali
The Luminare and Lighthouse trials are large and long studies designed to assess whether this reduction in LRRK2 activity can result in slowing long-term progression of the disease. The initiation of these two studies in 2022 was the culmination of a lot of research and a very exciting development for the Parkinson’s community (Click here to read a SoPD post on this topic). And there are more late-stage clinical trials targeting biological mechanisms believed to be underlying the condition (such as the Phase 3 trial of ambroxol which will start in 2023).
3. New GBA1/GCase insights
About 5-10% of the Parkinson’s population carry a genetic variation in a region of DNA called the GBA1 gene. The GBA1 gene provides the instructions for making an enzyme called GCase, which is involved in the waste disposal system of cells. This enzyme functions within small bags of enzymes – called lysosomes – that are used to break down old proteins.
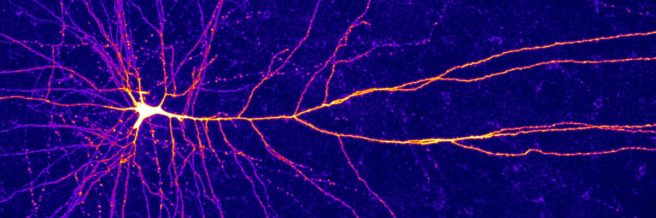
People with GBA1-associated Parkinson’s have a dysfunctional form of GCase, which results in reduced levels of GCase activity and this disrupts lysosomal activity. In a new report in 2022, scientists reported that the dysfunctional form of the GCase protein can be transported to lysosomes, but rather than failing to function inside the lysosome, it gets trapped on the outer surface of these small bags of enzymes.
The new research found that not only does GCase get stuck on the outer surface of lysosomes, but it blocks the entrance of other proteins – those that are being disposed of. This action results in a build up of waste outside of the lysosome, including proteins like alpha synuclein and Tau. This finding may be highlighting new biology and could help to explain several important features of GBA1-associated Parkinson’s (Click here to read a SoPD post about this topic).
# # # # # # #
The three pieces of research news above were what grabbed my attention the most in 2022, but it was a very full year of new data. Below, we’ll go month-by-month and discuss some of the other highlights.
Let’s begin with:
1. A new function for alpha synuclein:
In January, researchers reported that the Parkinson’s-associated protein alpha synuclein is required for the induction of some immune responses. They found that endogenous alpha synuclein is required for the induction of peritonitis (inflammation of the tissue in the peritoneum of the gut) by bacterial proteoglycan (in mice). Their study showed that alpha synuclein is generated and secreted at the sites of inflammation, and it promotes phenotypic & functional maturation of immune cells (dendritic cells). The researchers reported that “neural cells are the sources of alpha synuclein required for immune competence“, and they suggest that their data “supports the hypothesis that alpha synuclein accumulates within the nervous system of Parkinson’s individuals because of an inflammatory/immune response” (Click here to read more about this, click here to read the press release, & click here for a good write up on this research from Science Magazine. You can also click here to read an SoPD post on the topic).
2. Cell transplantation in the Copper state?
Sounds like some interesting developments are afoot at the Biodesign Institute at Arizona State University – the Michael J Fox Foundation has awarded $5.2M in grants to explore 3 pioneering treatments for Parkinson’s which will be conducted at the ASU-Banner Neurodegenerative Disease Research Center. Of particular interest, one of the projects will be a clinical trial for transplanting human iPSC derived dopamine neurons into the brains of patients with early onset autosomal recessive Parkinson’s due to Parkin mutations. This project will be in collaboration with the van Andel institute and Fujifilm Cellular Dynamics (Click here to read more about this).

3. Exercise!
A new observational cohort study of 237 early Parkinson’s patients found maintenance of high regular physical activity levels & exercise habits was associated with better clinical course of PD. Interestingly, each type of physical activity was associated with different effects (Click here to read more about this & click here to read the press release).
1. When I travel, I take everything I need
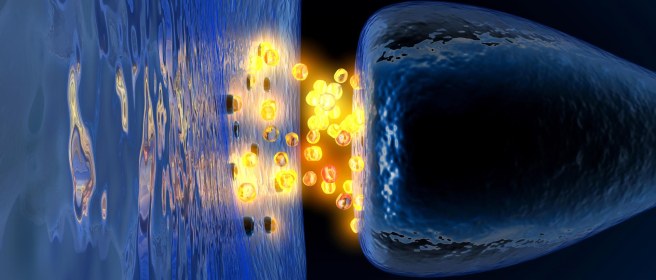
In February, researchers reported that mitochondria (the bean-shaped power stations of cells) can transport necessary mRNA on their outer surface when they move around cells. This action (via a mechanism involving SYNJ2BP and synaptojanin 2) allows for local translation of Pink1 and mitophagy (disposal of mitochondria) wherever it is required within neurons (Click here to read more about this).
2. Going really small to tackle LRRK2
Researchers presented data proposing (llama-derived) nanobodies as allosteric modulators of Parkinson’s–associated LRRK2. “In contrast to current type I kinase inhibitors, the studied kinase-inhibitory nanobodies did not induce LRRK2 microtubule association”. “These nanobodies inhibit LRRK2 via a mechanism that differs from the commonly used LRRK2 kinase inhibitors. Importantly, some of these nanobodies selectively inhibit certain LRRK2 activities (such as Rab phosphorylation) while leaving other activities (autophosphorylation) unaffected”. Could llama-derived nanobodies be a new class of therapeutic for Parkinson’s? (Click here to read more about this).
1. The NADPARK study results:
On the 1st of March, Norwegian researchers presented the results of the NADPARK study: A randomized phase I clinical trial of nicotinamide riboside supplementation in Parkinson’s; This was a small pilot (n=30) and the scientists reported that oral nicotinamide riboside (1,000mg/day for 30 days) treatment was well tolerated and led to significant (but variable) increase in cerebral NAD levels (measured by MRS imaging & cerebrospinal fluid measurements); nicotinamide riboside also decreased levels of inflammatory cytokines in blood & cerebrospinal fluid. These results provide further support and justification for the much larger, on going Phase II “NO-PARK study” (NCT03568968 – click here to read more about this, click here to read the press release associated with this study, and click here to read a SoPD post on this topic).

2. The silver linings of Parkinson’s:
Another interesting paper published in March involved scientists and Parkinson’s research advocates sharing the results (& interpretations) of an online exploratory survey asking if there are any “silver linings to having Parkinson’s” – a tough question, but a very powerful paper with some surprising and creative responses (Click here to read more about this and click here to read a SoPD post about this report).
3. A difference in identity?:
A research paper in March reported “a glutamatergic identity in dopamine neurons may be part of a neuroprotective response in Parkinson’s”. The researchers involved found that the glutamatergic-associated protein, VGLUT2, can be increased in some dopamine neurons in response to injury, and this appears to protect those cells. They also reported that an analysis of postmortem PD brains further supported this idea (Click here to read more about this).
1. It’s not just dopamine:
In April, German researchers reported that GABAergic neurons (generated by CRISPR-mediated direct in vivo reprogramming of striatal astrocytes) rescues voluntary motor behavior in a neurotoxin-induced mouse model of Parkinson’s. The reprogramming factors involved were Ascl1, Lmx1a, & Nr4a2. Two different investigative approaches have been used, and in both systems, a significant reduction of motor impairments was observed. The reprogrammed neurons did not acquire dopaminergic fate, suggesting “a novel intervention strategy beyond the restoration of dopamine levels” (Click here to read more about this).
2. The liraglutide results:
The initial results of the Phase 2 clinical trial exploring the diabetes medicine liraglutide in Parkinson’s were announced. In this Cure Parkinson’s supported study, the investigators found that 1 year of treatment with this drug resulted in improvements in non-motor symptoms, activities of daily living and quality of life measures. These encouraging insights into the effectiveness of this class of treatment builds on an increasing collection of data pointing towards GLP-1 receptor agonists as a useful new treatment for PD (Click here to read more about this and click here to read a SoPD post about this topic).
3. The UK Parkinson’s Disease Clinical Studies Group:
The UK Parkinson’s Disease Clinical Studies Group (UK PD-CSG) was launched this month. The group has been set up to develop and support Parkinson’s clinical research across the UK, with a special emphasis on studies exploring disease modification. In addition, the organisation will be encouraging patient education and engagement, as well as the training of future generations of researchers (Cure Parkinson’s is providing funding support to this group).
1. MODAG’s Phase Ib results:
The results of a Phase 1b randomised, double-blind, placebo-controlled clinical trial evaluating the safety, tolerability & pharmacokinetics of MODAG’s alpha synuclein oligomer modulator anle138b (which is being developed for Parkinson’s) were published. The treatment was safe and well tolerated at doses that were efficacious in preclinical studies. Roll on Phase 2! Cure Parkinson’s supported recruitment efforts for this Phase 1 work (Click here to read more about this).
2. A positive Phase III result for Amyotrophic lateral sclerosis:
A Phase 3 randomized clinical trial that enrolled 130 participants with early-stage ALS & moderate progression rate reported that ultrahigh-dose methylcobalamin (vitamin B₁₂) significantly slowed progression (ALSFRS-R total score) over a 16-week study. The ALSFRS-R total score at week 16 of the randomized period was 1.97 points greater with methylcobalamin (50 mg) than placebo (−2.66 vs −4.63; 95% CI, 0.44-3.50; P = .01). There were no differences in adverse events between groups. What was the potential mechanism of action behind this effect? Methylcobalamin/VitB12 plays a role in removing homocysteine (the build up of which is believed to be toxic), and blood homocysteine levels are increased in ALS, so perhaps high dose VitB12 may be reducing it (Click here to read more about this).
3. Improved characterisation of dopamine neuron subpopulations:
Researchers collected postmortem midbrain tissue from 8 control donors & performed single cell sequencing, identifying 10 populations of dopamine neurons. Using macaque midbrains, they spatially localized each within the substantia nigra pars compacta. Next they performed similar analysis on samples of brains from Parkinson’s & Lewy body dementia postmortem cases. Transcriptional changes in cells that expressed AGTR1 (the gene for angiotensin II receptor type 1 (AT1 receptor) point towards several canonical cell stress pathways (TP53 and NR2F2) as important to the process of PD-associated neuronal death (Click here to read more about this and click here to read the editorial).
1. Parkin becomes more inflammatory:
Parkinson’s has been shown to be associated with inflammatory responses by the immune system. NLRP3 is a protein involved in inflammation and researchers have just demonstrated that the Parkinson’s-associated protein Parkin binds to NLRP3 and keeps it at bay. Loss or reduction of Parkin primes & activates an inflammatory structure called the NLRP3 inflammasome in dopamine neurons. The scientists also found that the accumulation of another protein (called PARIS) due to Parkin loss also drives the activation of the NLRP3 inflammasome (Click here to read more about this).
2. The modification of acidification:
Lysosomes are a key component of the cellular waste disposal system. Researchers have reported that the Parkinson’s-associated protein TMEM175 is a highly proton-selective channel in the membrane of lysosomes that modulate the acidity of the inner environment of these tiny bags of enzymes. Deficiency in TMEM175 resulted in lysosomal over-acidification, which impaired the disposal/recycling of old proteins & the accumulation of alpha synuclein aggregation models of Parkinson’s (Click here to read more about this and click here to read an SoPD post on this topic).
3. Time to plan for a sartan?
In a new study, researchers reported that angiotensin type-1 (AT1) receptor & angiotensin-converting enzyme 2 (ACE2) serum autoantibodies were higher in 117 individuals with Parkinson’s (vs 106 controls). Crucially, AT1 autoantibodies increased neurodegeneration in cell culture conditions, and also increased levels of neuroinflammation markers. This situation was prevented by treatment with the AT1 antagonist candesartan. Of particular interest, AT1 autoantibodies were also found in the cerebrospinal fluid of people with Parkinson’s. Further support for repurposing angiotensin type-1 receptor blockers for Parkinson’s? (Click here to read more about this and click here to read an SoPD post on this topic).
1. Is alpha synuclein ‘interferon’ with the immune response?:
Researchers reported that Parkinson’s-associated α-synuclein is required for neuronal expression of interferon-stimulated genes (in response to viral infection). Curiously, when neurons that do not have α-synuclein are treated with type 1 interferon, they failed to induce a broad range of interferon stimulated genes, suggesting that α-synuclein interacts with type 1 interferon signaling. In addition, interferon-mediated phosphorylation of STAT2 is also dependent on α-synuclein. The researchers also looked at postmortem brain tissue from people with Parkinson’s (Click here to read more about this & click here to read an OPEN ACCESS version of the report).
2. Treadmills, PPARα, and fenofibrate:
Researcher reported that treadmill exercise reduced the spread of α-synuclein aggregation pathology in aged genetically engineered (A53T) mice. They determined that this effect resulted from the activation of Peroxisome proliferator-activated receptor alpha (PPAR-α) which stimulated lysosomal biogenesis (via TFEB). Interestingly when the researchers treated mice with fenofibrate – a PPARα agonist – in the absence of exercise, it also reduced α-synuclein aggregation pathology (Click here to read more about this).
3. Does Yerbe mate matter?
A multicenter case-control study across 3 countries (Argentina, Paraguay, & Uruguay) found an association between Yerba mate tea concentration per serving and lower risk of developing Parkinson’s (Click here to read more about this and click here to read a SoPD post on the topic).
1. Diet and fitness matter
A new “cohort study showed that a better diet quality & a higher level of physical activity were inversely associated with mortality risk among men & women with Parkinson’s“. A healthy diet & engaging in physical activity/exercise matters – “The current study also suggests that a healthy diet & higher levels of recreational physical activity may accomplish what medical intervention thus far has not been able to do: slow the pace of progression” (Click here to read more about this and click here to read the editorial about this research).

2. While you were sleeping
Researchers at Massachusetts Institute of Technology reported artificial intelligence-enabled detection & assessment of Parkinson’s using nocturnal breathing. Low-cost, “Objective, noninvasive, at-home assessment“. The study also suggests that the “AI model may be useful for risk assessment before clinical diagnosis” (Click here to read more about this and click here to read the press summary about this research).

3. The Lords of LRRK – 2 papers
The Lords of LRRK present XL01126: A fast-acting, cooperative, selective, orally bioavailable, brain penetrant PROTAC degrader of Parkinson’s-associated LRRK2; “An attractive starting point for future drug development” (Click here to read more about this). Another new paper explored the impact of 100 LRRK2 variants linked to Parkinson’s on kinase activity & microtubule binding – if you like blots, this one is for you! A tour de force; The “findings will stimulate work to better understand the mechanisms by which variants impact biology & provide rationale for variant carrier inclusion/exclusion in ongoing & future LRRK2 inhibitor clinical trials” (Click here to read more about this).
1. More data indicating that Terazosin reduces the risk of Parkinson’s
New data found that men using Terazosin/doxazosin/alfuzosin have a somewhat lower risk of developing Parkinson’s than those using tamsulosin & a slightly lower risk than those using 5α-reductase inhibitors. These data provide further support for current efforts exploring the repurposing of terazosin for Parkinson’s (Click here to read more about this).
2. Is the melanoma mystery solved?
We have known for a long time that people with Parkinson’s have a higher risk of developing melanoma and vice versa. But now researchers have identified an interesting connection. A new report finds that both endogenously produced DOPA & L-DOPA/carbidopa (the FDA-approved therapy for PD) inhibit the muscarinic acetylcholine receptor M1 (CHRM1) in darkly pigmented melanocytes & this inhibits the growth of melanoma both in cell culture and in mice (Click here to read more about this and click here to read a previous SoPD post on this topic).
3. A history of infections
Hospital-treated infections in early- & mid-life was investigated for its risk of Alzheimer’s and Parkinson’s later in life. A nationwide nested case-control study from Sweden found “Hospital-treated infections, especially in early- & mid-life, were associated with an increased risk of AD & PD“. The results “suggest that infectious events may be a trigger or amplifier of a preexisting disease process, leading to clinical onset of neurodegenerative disease at a relatively early age“, but “the results do not formally prove a causal link” (this was an observational study only – Click here to read more about this).
4. Forget about wearables, think: “Invisibles”
Using radio waves from a wall mounted device, MIT researchers continuously monitored 50 participants, with & without Parkinson’s, in their homes for up to 1 year. The system could accurately track decline in gait and the effects of the COVID lockdowns (Click here to read more about this and click here to read a previous SoPD post about this topic).
1. New cell transplantation study launched:
Swedish authorities have granted approval for a clinical trial of stem cell-derived cell transplantation therapy for the treatment of Parkinson’s. The trial – called STEM-PD – will involve recruiting a total of 8 patients for transplantation, starting with participants in Sweden, and with subsequent plans for enrolment of patients in Cambridge, UK (Click here to read more about this).
2. Mitochondria. Always mitochondria:
Researchers in Sweden reported that Parkinson’s is associated with a 20% lower number of mitochondrial DNA copies, but 26% longer telomeres (in blood vs controls). Telomere length in blood positively correlated with medication (L-dopa) & disease duration. In the brain, Parkinson’s, PD dementia & Dementia with Lewy Bodies case “showed (46–95%) depleted mtDNA copies, but (7–9%) longer telomeres” vs controls. Plus, lower mitochondrial biogenesis (PGC-1α & PGC-1β) & higher load of a cellular senescence marker in postmortem CNS tissue (Click here to read more about this).
3. Neflamapimod presents encouraging results:
Preclinical & randomized clinical evaluation (NCT04001517) of the p38α kinase inhibitor neflamapimod in mild-to-moderate dementia with Lewy bodies presented encouraging results. Preclinical testing of agent protected neurons in a model of basal forebrain cholinergic degeneration. And then in a clinical pilot study (N=91, 16-weeks of treatment, double-blind study), neflamapimod did not show an effect on the primary endpoint (a cognitive-test battery), but on secondary endpoints (a measure of functional mobility & a dementia rating-scale) improvements were observed (Click here to read more about this).
1. The STAT-PD clinical trial results:
Publication of the JP Moulton/Cure Parkinson’s supported STAT-PD study results:
A 2-year evaluation of simvastatin in 235 individuals with Parkinson’s reports that the treatment did not have a disease-modifying effect; This was a randomized, double-blind, parallel-group, placebo-controlled futility analysis conducted across 23 sites within the UK; Primary end point was MDS-UPDRS part III score measured while not on meds; More information on the trial can be found by clicking here. Cure Parkinson’s was a funder of this clinical trial (Click here to read the results).
2. Autophagy promotes cell survival by maintaining NAD levels:
New research demonstrated an evolutionarily conserved role for autophagy in cell survival by maintaining nicotinamide adenine dinucleotide (NAD) levels. Scientists demonstrated that uncontrolled depletion of the NAD ultimately contributed to mitochondrial membrane depolarization & cell death. Normal levels of autophagy is required to keep NAD-targeting enzymes like PARP and Sirtuin families in check (Click here to read more about this).
3. Can a fiber-rich diet influence microglial function?:
New research in mice found that a fiber-rich diet can influence microglial function in a preclinical model of Parkinson’s. Mice producing high levels of Parkinson’s-associated α-synuclein had reduced motor deficits and less α-synuclein aggregation when placed on a high fiber diet. And the effect was specific to microglia because depletion of microglia (using a CSF1R inhibitor) eliminated the effect (Click here to read more about this).
1. The deferiprone clinical trial results
The results of the large phase 2 FAIRPARK II study evaluating the iron chelator deferiprone in 372 recently diagnosed, non-Levodopa treated cases of Parkinson’s (186 on deferiprone and 186 on placebo over a period of 36 weeks), indicated that symptoms were worse for those treated with deferiprone compared to placebo. Progression of symptoms leading to the initiation of dopaminergic therapy occurred in 22.0% of the participants in the deferiprone group compared with just 2.7% of those in the placebo group (Click here to read more about this)
2. Sigma 1 again
Anavex Life Science‘s sigma 1 agonist Blarcamesine has met both primary & secondary endpoints in their randomized, double-blind, multicenter, placebo-controlled Phase 2B/3 clinical trial in Alzheimer’s. This study involved 509 participants who were randomised (1:1 ratio) to treatment with Blarcamesine or placebo for 48 weeks. The agent was safe & well tolerated, and a treatment difference in mean score change of -1.85 points on ADAS-Cog (p=0.033) was reported (Click here to read more about this)
3. Results from another exenatide clinical trial
Korean biotech firm Peptron announced that they observed no statistical significance between the treatment & placebo groups (for the mean change of MDS-UPDRS part 3 score) in a Phase 2 study investigating their GLP-1R agonist PT320 in 99 people with Parkinson’s. The company did announced that they saw statistically positive secondary outcomes that were encouraging enough for them to continue developing the agent (Click here to read more about this)
And that is it. Those were some of the pieces of Parkinson’s research that grabbed our attention here at SoPD HQ in 2022.
So what does it all mean?
I don’t know about you, but I am glad to see the back of 2022.
And I look forward to a happier 2023.
The next SoPD post is usually the annual “Road Ahead” post, but unfortunately I am going to have to skip it this year. It is an extremely time consuming project to put together, and due to circumstances out of my control I simply do not have the capacity this year to provide it.
I am sorry for this, but I will hopefully be able to make up for it next year. Fingers crossed.
Happy new year to all!
 All of the material on this website is licensed under a
All of the material on this website is licensed under a
Creative Commons Attribution 4.0 International License
You can do whatever you like with it!
The banner for today’s post was sourced from Youtube











































Seems like a lot of good news – particularly about GABA. My neurologist recently put me on muscle relaxants that work on gaba-A and gaba-B, They seem just as important to me as CD/LD.
LikeLike
Simon, Good to see SoPD is back, I find it very useful.
Have become interested in GlcNAc as a putative intervention against asyn prion-like progression. Bw Peter
LikeLike
Simon. Really appreciate your efforts in posting this material in adversity. It really casts a ray of sanity in all that is going on. Keep up the good work.
LikeLike