|
# # # # For a long time, researchers have recognised that there is an association between melanoma and Parkinson’s – with individuals affected by either condition being at higher risk of developing the other. The underlying biology of this connection has remained a mystery. Recently, new data has pointed toward an unlikely bridge between the two, in the form of DOPA – a key ingredient in the production of the chemical dopamine. In today’s post, we will discuss what melanoma is, explore the connections with Parkinson’s, and review the new research on DOPA. # # # # |
 Godzone (Noun). Source: Mindfood
Godzone (Noun). Source: Mindfood
Growing up in New Zealand, the author of this blog developed a healthy fear of the dangers of melanoma at a very young age.
Unfortunately, New Zealand has one of the highest age-standardised incidence rates of melanoma in the world. It occurs in approximately 50 people per 100,000 of the general population, each year (it is one of many things we beat Australia at, their incidences is only 48 per 100,000).
By contrast, in the US the incidence is just 21.8 per 100,000 (Source).
And despite being less common than other types of skin cancer, in New Zealand melanoma accounts for 80% of skin cancer-related deaths (Source).
Wow! Really?
Really, really.
Fact: Melanoma is the third most common cancer in men and women in New Zealand (Source – in the UK and US, it is 5th).
But why the high incidence?
Ultraviolet radiation is the main reason. New Zealand and Australia have ~40% higher levels of ultraviolet radiation than the northern hemisphere. That whole ozone hole thing above Antarctica – yep, it’s still a thing (source).
Combine that unfortunate circumstance with the fact that both countries have a high proportion of antipodeans with lighter pigmented skin making up their populations – who (I can confirm) are more susceptible to sunburn – and you have a perfect recipe for melanoma.
I can remember as a kid returning home from the beach looking like a boiled lobster… on a regular basis.
 An ACDC fan. Source: Runt
An ACDC fan. Source: Runt
I really hate to say it, but New Zealand isn’t quite perfect.
Interesting, but what does this have to do with Parkinson’s?
A lot.
You see, Parkinson’s has a very strange relationship with melanoma.
As we have stated in previous SoPD posts (Click here, here, here and here to read those posts) people with Parkinson’s disease are 2-8 times more likely to develop melanoma than people without Parkinson’s. It is not something to stress about, but it is wise to be mindful of and if there are any funny looking spots on your body, why not get them checked out.
And this association between Parkinson’s and melanoma has been replicated once or twice (Click here, here, here, here, here, here, here, here, here, here, here, here, here, here, and here to read studies supporting the statement that melanoma risk is higher among individuals with Parkinson’s).
The truly baffling detail in this story, however, is that this relationship is reciprocal – if you have melanoma you are almost 3 times more likely to develop Parkinson’s than someone without melanoma (Click here and here to read more about this).
Que?!?
Yeah, it’s a real mystery. One of those riddles, wrapped in a mystery, inside an enigma situations.
Fascinating. But what is melanoma exactly?
Melanoma is a type of skin cancer.
It develops from the pigment-containing cells known as melanocytes. Melanocytes are melanin-producing cells located in the bottom layer (the stratum basale) of the skin’s outer layer (or epidermis).

The location of melanocytes in the skin. Source: Wikipedia
Melanocytes produce melanin, which is a pigment found in the skin, eyes, and hair. It is also found in the brain in certain types of cells, such as dopamine neurons (where it is referred to as neuromelanin).

Neuromelanin (brown) in dopamine neurons. Source: Schatz
Melanomas are usually caused by DNA damage resulting from exposure to ultraviolet radiation. Ultraviolet radiation from tanning beds increases the risk of melanoma (Source), as does excessive air travel (Source), or simply spending to much time sun bathing.
Approximately 2.2% of men and women will be diagnosed with melanoma at some point during their lives (Source). In women, melanomas most commonly occur on the legs, while in men they are most common on the back.
Generally, melanomas is one of the safer cancers, as it can usually be detected early by visual inspection. This cancer is made dangerous, however, by its ability to metastasize (or spread to other organs in the body).

The stages of melanoma. Source: Pathophys
So how are Parkinson’s and melanoma connected? Are there any genetic associations between them?
No.
When the common genetics mutations that increase the risk of both conditions were previously analysed, it was apparent that none of the known Parkinson’s mutations make someone more susceptible to melanoma, and likewise none of the melanoma-associated genetic mutations make a person vulnerable to Parkinson’s (Click here, here, and here to read more about this).
In fact, researchers have only found extremely weak genetic connections between two conditions (Click here to read our previous post on this).
Like we were saying: it’s a real mystery.
Are there any other known connections between Parkinson’s disease and melanoma?
Yes.
Another shared feature of both Parkinson’s and melanoma is the build up of a protein called alpha synuclein. Alpha synuclein is believed to be one of the villains in Parkinson’s – building up inside a cell, becoming toxic, and eventually killing that cell.
But researchers have noticed that melanoma also has a build up of alpha synuclein, but those cells don’t die:

Title: Parkinson’s disease-related protein, alpha-synuclein, in malignant melanoma
Authors: Matsuo Y, Kamitani T.
Journal: PLoS One. 2010 May 5;5(5):e10481.
PMID: 20463956 (This article is OPEN ACCESS if you would like to read it)
In this study, researchers found that alpha synuclein was detected in 86% of the primary and 85% of the metastatic melanoma (the protein is not detectable in the non-melanoma cancer cells or normal skin).
And other researchers have replicated this finding and discovered something interesting about alpha synuclein and melanoma – the protein protects the cancer cells from dying.
They published their findings in this report:

Title: Treatment with diphenyl-pyrazole compound anle138b/c reveals that α-synuclein protects melanoma cells from autophagic cell death
Authors: Turriani E, Lázaro DF, Ryazanov S, Leonov A, Giese A, Schön M, Schön MP, Griesinger C, Outeiro TF, Arndt-Jovin DJ, Becker D
Journal: Proc Natl Acad Sci U S A. 2017 Jun 20;114(25):E4971-E4977.
PMID: 28584093 (This report is OPEN ACCESS if you would like to read it)
In their study, the researchers looked at levels of alpha synuclein in melanoma cells and they treated those cells with a drug called anle138b. This drug is being developed by the biotech company MODAG for use in Parkinson’s.
Anle138b has been shown to inhibit the accumulation of alpha synuclein in models of Parkinson’s and it is now in clinical testing (Click here to read more about this).
When the investigator treated their melanoma cells with anle138b, they observed something fascinating: the cell morphology (or physically) changed, leading to massive melanoma cell death.
The investigators found that this cell death was caused by instability of mitochondria and a major dysfunction in the autophagy process.
What does that mean?
Mitochondria, you may recall, are the power house of each cell. They keep the lights on. Without them, the lights go out and the cell dies.
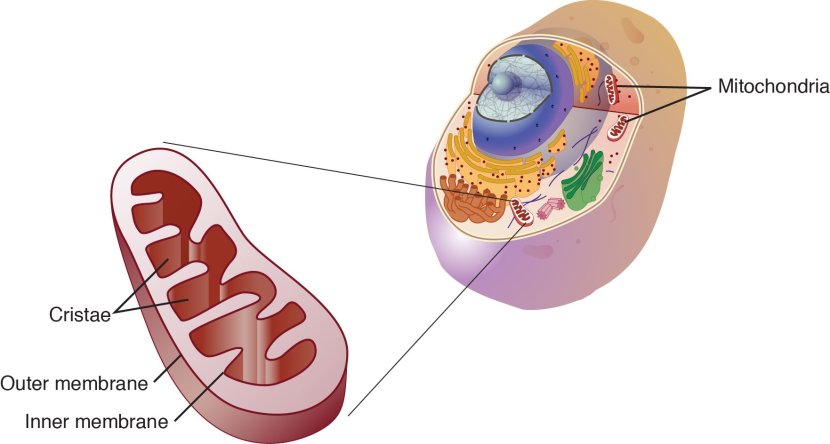
Mitochondria and their location in the cell. Source: NCBI
And autophagy is the garbage disposal/recycling process within each cell, which is an absolutely essential function. Without autophagy, old proteins and mitochondria will pile up making the cell sick and eventually it dies. Through the process of autophagy, the cell can break down the old protein, clearing the way for fresh new proteins to do their job.

The process of autophagy. Source: Wormbook
Waste material inside a cell is collected in membranes that form sacs (called vesicles). These vesicles then bind to another sac (called a lysosome) which contains enzymes that will breakdown and degrade the waste material. The degraded waste material can then be recycled or disposed of by spitting it out of the cell.
What the researchers treating their cells with anle138b found was that the high levels of alpha synuclein keep the mitochondria stable and the autophagy process working at a level that helps to keeps the cancer cell alive.
They next replicated this cell culture research in mice with melanoma tumors. When the mice were treated with anle138b, the cancer became malformed and the autophagy process was blocked.
The researchers concluded that “alpha synuclein, which in PD exerts severe toxic functions, promotes and thereby is highly beneficial to the survival of melanoma in its advanced stages”.
Interesting. Is anle138b the only alpha synuclein-targeting drug that does this?
No.
Other alpha synuclein-modulating drugs have been shown to impact melanoma though. For example, the tricyclic antidepressant nortriptyline has been reported to have anti-cancerous properties on melanoma cell lines (Click here to read more about this.
It is not clear if nortriptyline’s activity on alpha synuclein was playing a role in this previous melanoma research, but it is a curious coincidence (Click here to read a previous SoPD post on nortriptyline).
So alpha synuclein is the link between melanoma and Parkinson’s?
Perhaps.
But very recently another intriguing link has been discovered. And the finding was published in this report:
 Title: Endogenous DOPA inhibits melanoma through suppression of CHRM1 signaling.
Title: Endogenous DOPA inhibits melanoma through suppression of CHRM1 signaling.
Authors: Doepner M, Lee I, Natale CA, Brathwaite R, Venkat S, Kim SH, Wei Y, Vakoc CR, Capell BC, Katzenellenbogen JA, Katzenellenbogen BS, Feigin ME, Ridky TW.
Journal: Sci Adv. 2022 Sep 2;8(35):eabn4007.
PMID: 36054350 (This report is OPEN ACCESS if you would like to read it)
In this very recently published study, the researchers reported that the naturally produced large neutral amino acid dihydroxyphenylalanine (or DOPA) has the ability to slow the growth and proliferation of melanoma (and even has resistance to the oncogenic effects of the major human melanoma oncoprotein BRAF(V600E).
What does any of that mean?
Dihydroxyphenylalanine is an amino acid (the building blocks of proteins). It comes in two forms: D-3,4-dihydroxyphenylalanine and L-3,4-dihydroxyphenylalanine.
 L-3,4-dihydroxyphenylalanine. Source: Wikipedia
L-3,4-dihydroxyphenylalanine. Source: Wikipedia
The second of these forms should be well known to most people with Parkinson’s. L-3,4-dihydroxyphenylalanine is also known as L-DOPA or levodopa.
Dihydroxyphenylalanine is an intermediate in the production of many important players in the biochemistry of life (critically for us: the chemical dopamine):
 Source: Sciencedirect
Source: Sciencedirect
Not highlighted in the image above is the fact that dihydroxyphenylalanine is also involved in the production of melanin (the pigment we mentioned towards the top of this post).
So, this stuff DOPA – which is an ingredient in the production of both dopamine and melanin – can slow the growth of melanoma?
Yes.
Ok. How did they discover that?
The discovery came about when the researchers noticed that darkly coloured melanoma cells (meaning they have lots of melanin pigmentation) grow twice as slowly as lightly coloured melanoma cells. Through a series of manipulations, they found that nothing they did externally altered this phenomenon, so they concluded that something intrinsic (inside the cells) must be influencing this difference in rate of growth.
They turned their focus on melanin.
The description of melanin up at the top of this post was rather simplistic. The synthesis of melanin occurs through a complex multistep process, which is regulated by over 200 different genes.
But key to all of it is dihydroxyphenylalanine (or DOPA).
The researchers noted that the darkly pigmented melanoma cells contained approximately 300% more DOPA than their lightly pigmented, faster growing counterparts.
So they decided to test the crazy idea that maybe DOPA is inhibiting the growth of the darkly pigmented melanoma cells. They did this by exposing darkly pigmented melanoma cells and lightly pigmented, faster growing melanoma cells to different amounts of DOPA.
And guess what happened….
The DOPA treatment had no effect on the darkly pigmented melanoma cells, but it decreased the proliferation rate of lightly pigmented melanoma cells in a dose-dependent fashion (meaning the higher the dose, the slower the growth). This observation suggested to the researchers that DOPA is a major determinant of proliferative differences in melanoma cells.
And while these initial experiments were conducted in cell culture, the investigators found that DOPA also slowed the proliferation of melanoma cells in mice as well.
Given the dose-dependent decrease in proliferation rate of melanoma cells to DOPA, the researchers assumed that the action of DOPA must be mediated by a specific receptor. So they conducted a series of experiments which eventually pointed towards the muscarinic acetylcholine receptor M1 (CHRM1), and they were able to identify a specific biological pathway by which DOPA was having its effect.
 Source: Science
Source: Science
And this represented a previously unidentified, but druggable set of targets for future melanoma therapies. Of particular interest in this situation is that the DOPA effect even worked on cells carrying major human melanoma-associated genetic mutations (such as BRAF-V600E).
And before you ask: No, the CHRM1 gene is not associated with Parkinson’s.
So the treatment that we use for Parkinson’s (levodopa) could be slowing down the proliferation of melanoma?
That is what the data suggests.
Does that mean that taking levodopa decreases the incidence of melanoma?
For a long time, there has been speculation around the idea that levodopa could actually be increasing the risk of melanoma in Parkinson’s, because levodopa is involved with the production of melanin.
But there is data supporting the idea that DOPA could be reducing the incidence of melanoma..
In 2017 this report was published:
 Title: Parkinson Disease and Melanoma: Confirming and Reexamining an Association.
Title: Parkinson Disease and Melanoma: Confirming and Reexamining an Association.
Authors: Dalvin LA, Damento GM, Yawn BP, Abbott BA, Hodge DO, Pulido JS.
Journal: Mayo Clin Proc. 2017 Jul;92(7):1070-1079
PMID: 28688464 (This report is OPEN ACCESS if you would like to read it)
In this study, the researchers conducted a retrospective cohort investigation examining the association between melanoma and Parkinson’s, and they concluded that people with Parkinson’s had a 3.8-fold increased risk of having melanoma, while melanoma patients had a 4.2-fold increased probability of developing Parkinson’s (compared to controls). Given the difference in frequency between these two groups, this finding argues against any role for levodopa in increasing melanoma risk.
It could also suggest that once diagnosed and taking levodopa, the rate of melanoma may decrease. Further research is required before we can make too many speculations in this direction.
So what does it all mean?
I have long scratched my badly scarred head (from too many years of exposure to the harsh southern hemisphere sun) contemplating the curious relationship between melanoma and Parkinson’s. It is a jigsaw puzzle that fascinates me. And this recent report suggesting that levodopa – the medication that is used to treat Parkinson’s – can slow the growth of melanoma cells, provides another twist in the tale that helps to keep me hooked.
It will be interesting to see if this new result can be independently replicated and if so, whether further investigations will point toward Levodopa or CHRM1 pathway-related agents can be targeted towards melanoma. While this may not have direct implications for the treatment of Parkinson’s, I thought the science was interesting and worthy of a post.
 All of the material on this website is licensed under a
All of the material on this website is licensed under a
Creative Commons Attribution 4.0 International License
You can do whatever you like with it!
ADDENDUM: 26th November 2022
One additional piece of research associated with this story. Today an interesting report was published describing the clinicopathologic characteristics of melanoma in people with Parkinson’s.
This is the report:
 Title: Clinicopathologic Characteristics of Melanoma in Parkinson’s Disease Patients
Title: Clinicopathologic Characteristics of Melanoma in Parkinson’s Disease Patients
Authors: Flynn MS, Robinson C, Patel S, Liu B, Green C, Pavlis M,
Journal: JID Innovations, 2022, 100173
PMID: N/A (This report is OPEN ACCESS if you would like to read it)
In this study, the researchers at Duke University reported that 70 cases of individuals who had been diagnosed with both Parkinson’s and melanoma (between January 1st, 2007 to January 1st, 2020). They compared these cases with 102 age-, sex-, and race-matched control individuals who did not have Parkinson’s, but did have melanoma.
Interestingly, the head and neck regions accounted for approximately 40% of invasive melanomas in the Parkinson’s group (compared to just 25% in the control group). And when the researchers looked at metastatic melanomas, they found that half of metastatic cases in the Parkinson’s group originated on the head and neck.
So keep an eye out for any funny dark spots on the head and neck region.
The banner for today’s post was sourced from News-medical


I was diagnosed with Parkinson’s over ten years ago. I have had melanoma three times prior to the diagnosis but not since which seems to concur with what you are saying. But, I also have psoriasis (another skin-related disease) which appears to increase the risk of getting Parkinson’s by 38% (Ungprasert P, Srivali N, Kittanamongkolchai W. Risk of Parkinson’s Disease Among Patients with Psoriasis: A Systematic Review and Meta-analysis. Indian J Dermatol. 2016 Mar-Apr;61(2):152-6. doi: 10.4103/0019-5154.177771. PMID: 27057013; PMCID: PMC4817438.) The good news is that they both have something to do with IL-17a and after asking my dermatologist if she could prescribe Cosentyx/Secukinumab, I was able to reduce my Parkinson’s meds by half. Skin and Parkinson’s seem to have many connections that might be worth pursuing.
LikeLike
Hi – I’m the primary author on the DOPA/CHRM1 paper. I really loved this post – you are able to eloquently disseminate complex science into everyday language. Thanks for highlighting my research 🙂
LikeLike