|
# # # # For a very long time, curcumin has been used as a nutritional and medicinal agent by many cultures. Very recently, a clinical trial was conducted to explore the potential of curcumin on Parkinson’s. And the findings were interesting. In today’s post, we will review the review the results of that study (and others). # # # # |
 Source: News-medical
Source: News-medical
Next time you are speaking with your neighbour, you should point out to them that there is a great deal of diversity in the number of species of Curcuma plants.
In India alone, there is approximately 40 to 45 species. And in Thailand there is another 30 to 40 species. Throughout tropical Asia there are numerous wild species of Curcuma, and even New Guinea and northern Australia are known to have Curcuma plants.
 Curcuma plants. Source: Pacificbulbsociety
Curcuma plants. Source: Pacificbulbsociety
Curcuma is a perennial, herbaceous flowering plant that belongs to the broader ginger family. The plants can reach a height of one meter and they produce numerous, edible rhizomes (creeping rootstalk).
 Rhizomes. Source: Etsy
Rhizomes. Source: Etsy
The interior of these rhizomes are yellow or orange and can be reduced into a powder.
That powder is the spice we call turmeric.
Great. But what does turmeric have to do with Parkinson’s?
We’ll come to that in a second. Bear with me for a moment.
The primary bioactive components of turmeric are molecules called curcuminoids. Only only 2 – 9% of turmeric is curcuminoids, and just one makes up approximately 75% of all the active curcuminoids.
That one is named curcumin.
 Source: PMC
Source: PMC
It was in 1815 that Henri Auguste Vogel and Pierre Joseph Pelletier first reported the isolation of a “yellow coloring-matter” from the rhizomes of turmeric that has gone on to be recognised as curcumin. But the use of turmeric dates back nearly 4000 years to the Vedic culture in India, and it has since been used by many cultures in cooking.
 Tumeric. Source: Cerebrum
Tumeric. Source: Cerebrum
Turmeric has also been recognised for its medicinal properties.
Much of therapeutic benefits of turmeric have been attributed to curcumin. It exhibits antioxidant, anti-inflammatory and anti-cancer properties, crosses the blood-brain barrier, and there are numerous studies that indicate neuroprotective properties in various models of neurological disorders.
Some of those neuroprotective properties may be due to the ability of curcumin to activate the NRF2 pathway (Click here , here and here for more on this).
What is the NRF2 pathway?
NRF2 is a protein that functions as a transcription factor.
What is a transcription factor?
A transcription is the process of converting (or transcribing) DNA into RNA. Small regions of DNA that provide the instructions for making a protein are called genes. Transcription factors – like the protein NRF2 – are activators of transcription. They bind to DNA next to specific genes and help to initiation the transcribing of the DNA into RNA.

An example of a transcriptional activator. Source: Khan Academy
So when NRF2 binds to certain regions of DNA, it aids in the production of the RNA for the nearby gene, which then results in specific proteins being produced.
And this is where NRF2 gets interesting.
You see, NRF2 binds to AREs.
What are AREs?
Antioxidant response elements (ARE) are regions of DNA commonly found beside genes that provide the instructions for various antioxidant and protective proteins. The ARE region of genes is the section of DNA where transcription is initiated for each gene. They are pieces of DNA that a transcription factor like NRF2 binds to and activates the production (or transcription) of RNA that provides the instructions for making proteins with antioxidant properties.
What does that mean? Antioxidant properties?
Oxidation is the loss of electrons from a molecule, which in turn destabilises that particular molecule. It is a process that is going on all around us – even within us.
Iron rusting is the example that is usually used to explain oxidation. Rust is the oxidation of iron – in the presence of oxygen and water, iron molecules will lose electrons over time. And given enough time, this results in the complete break down of objects made of iron.

Rusting iron. Source: Thoughtco
Oxidation also occurs in biology.
Molecules in your body go through the same process of losing electrons and becoming unstable. This chemical reaction leads to the production of what we call free radicals, which can then go on to damage cells.
What is a free radical?
A free radical is an unstable molecule – unstable because they are missing electrons. They react quickly with other molecules, trying to capture the needed electron to re-gain stability. Free radicals will literally attack the nearest stable molecule, stealing an electron. This leads to the “attacked” molecule becoming a free radical itself, and thus a chain reaction is started. Inside a living cell this can cause terrible damage, ultimately killing the cell.
Antioxidants are the good guys in this situation. They are molecules that neutralise free radicals by donating one of their own electrons. The antioxidant don’t become free radicals by donating an electron because by their very nature they are stable with or without that extra electron.

How free radicals and antioxidants work. Source: h2miraclewater
Given that antioxidants and protective proteins are generally considered to be a good thing for sick/dying cells, you can see why NRF2 is an interesting protein to investigate (Click here to read a previous SoPD post on this topic).
So curcumin activates the NRF2 pathway which results in antioxidants and protective proteins being produced?
In a nutshell, that is what the preclinical evidence suggests.
Is this all curcumin does?
No, it has been associated with lots of biological actions.
Of particular interest to us here is that it has been shown to prevent the clustering of alpha synuclein.
We talk about alpha synuclein a lot on this website. It is one of the most common proteins in the human brain, and many believe that it is centrally involved with the neurodegeneration associated with Parkinson’s.
The effects of aggregated Alpha Synuclein protein in a neuron. Source: R&D
Alpha synuclein has different functions in the brain – particularly in terms of communication between neurons. But in the Parkinsonian brain, for reasons that are still unknown to us alpha synuclein starts to clump (or ‘aggregate’) together (Click here to read a previous SoPD post about this). This aggregation is believed to play a role in the neurodegeneration associated with the condition, and it has been proposed that by stopping or slowing this aggregation we may be able to delay progression of Parkinson’s.
Curcumin has been reported to reduce the levels of alpha synuclein protein aggregation (click here and here for more on this).
For a good review on the other features of curcumin, you could have a look at this article.
|
# RECAP #1: Turmeric is a spice that is derived from the root of Curcuma plants. Most of the active component of turmeric is curcumin, which has numerous interesting properties – including reducing oxidation and inhibiting alpha synuclein targeting # |
Given these interesting properties, has curcumin ever been clinically tested in Parkinson’s?
Before we answer that question, there is one small detail regarding curcumin that we need to address and that detail is bioavailability.
What is bioavailability?
Bioavailability refers to the extent (and rate) that an active agent (like a drug) enters systemic circulation and can thereby achieve its intended action. It is a key indicator of drug absorption.
The big issue with curcumin is that it has very poor bioavailability. It is not very well absorbed into the body.
In fact, the vast majority of curcumin (more than 90%) consumed orally is excreted in feces (Click here to read more about this topic).
And poor bioavailability is an issue for a lot of molecules that have presented interesting properties in preclinical research. This has led researchers to develop new methods and formulations for getting molecules (like curcumin) into the body better so as to test their potential against conditions like Parkinson’s.
Understood. So has curcumin ever been clinically tested in Parkinson’s?
Yes, it has. Very recently the results of this clinical study were published:
 Title: The Effect of Curcumin on Idiopathic Parkinson Disease: A Clinical and Skin Biopsy Study.
Title: The Effect of Curcumin on Idiopathic Parkinson Disease: A Clinical and Skin Biopsy Study.
Authors: Donadio V, Incensi A, Rizzo G, Fileccia E, Ventruto F, Riva A, Tiso D, Recchia M, Vacchiano V, Infante R, Petrangolini G, Allegrini P, Avino S, Pantieri R, Mostacci B, Avoni P, Liguori R. J
Journal: Neuropathol Exp Neurol. 2022 Jun 20;81(7):545-552.
PMID: 35556131 (This report is OPEN ACCESS if you would like to read it)
In this study, the researchers recruited 19 individuals who were prepared to be treated with curcumin supplementation for 12 months and have a skin biopsy at baseline and at the end of the trial. They also recruited 14 additional people with Parkinson’s, who did not want to take the curcumin treatment, but were prepared to act as controls in the study (they would be assessed over the 12 month period while remaining on standard care, and prepared to have skin biopsies taken).
The participants taking curcumin took 1 gram of a product called Meriva twice per day (so 2 grams per day of curcumin in total) for 1 year. Meriva is a nano-delivery system of curcumin that uses phytosomes.
What are phytosomes?
Phytosomes (also known as phyto-phospholipid complexes) are tiny spherical sacs that are formed by a membrane and filled with liquid. They are very similar to liposomes, in that their membranes are made up of one or more bilayers, but phytosomes differ from liposomes in one key way: While liposomes carry their drug cargo within the middle of the sac, phytosomes carry their drug cargo within the membrane itself:
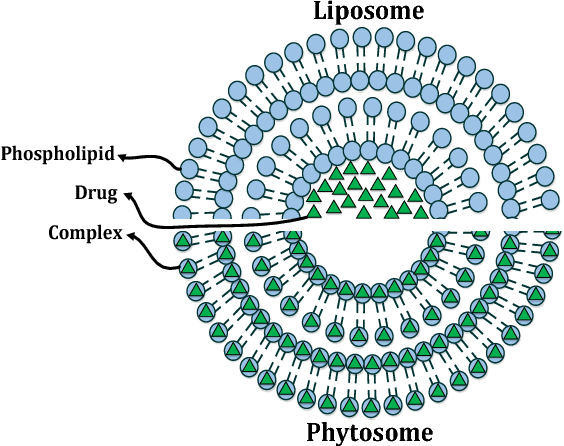 The difference between phytosomes and liposomes. Source: Semanticscholar
The difference between phytosomes and liposomes. Source: Semanticscholar
So Meriva is a product that contains phytosomes (which are spherical sacs that carry curcumin within their membranes). This delivery system is designed to improve the bioavailability of curcumin.
The trial involved clinical assessments assessing motor symptoms (measured using the MDS-UPDRS and H&Y clinical rating scales) as well as non-motor features (assessed by NMSS – a 30-item rater-based scale to assess a wide range of non-motor symptoms).
At baseline (the start of the study), the curcumin-supplemented group and the untreated patients showed no significant differences in terms of age, sex, and disease duration. The curcumin-treated group did show a slightly higher motor disability on their MDS-UPDRS scores, which corresponded to a higher L-dopa dosage.
After 12 months of assessment, the researchers found that the curcumin-treated group did not exhibit any serious adverse events from the treatment and the dietary supplementation was well-tolerated. The treated group had elevated detectable curcuminoid levels within the brain (based on measurement of cerebrospinal fluid), but that these were lower than measures made from blood. This suggested that curcumin was accessing the brain, but not to the same levels that were found in the blood. The untreated group showed no detectable traces of curcumin, curcuminoids, or their metabolites in their blood.
When the researchers looked at the UPDRS scores of the curcumin-treated group, they found that the increase in scores (indicating a worsening of symptoms) were less than those in the untreated group. And this is particularly interesting because one condition for being in the treatment group was that they were not allowed to increase their L-dopa medication over the 12 months of the study. By contrast, the untreated groups symptoms progressed slightly faster, and they increased their L-dopa by 150m/day on average.
 Source: PMC
Source: PMC
Also of interest, within the curcumin-treated group, participants with shorter disease duration (less than 6 years; N=9) had a better outcome than participants who had had Parkinson’s for a longer period of time (more than 6 years; N=10).
One detail in the results that I would like to point out is that at the end of the study (after 12 months of curcumin supplementation), the researchers reported decreases in cognitive scores (which bizarrely reflect improvements in mental ability) in the curcumin-treated group, compared to the opposite trend in the untreated group (whose scores increased – indicating a worsening of cognitive ability). This effect was apparent on two cognitive tests (the COMPASS-31 and NMSS – see graph above).
You mentioned that skin biospies were taken. Why did the researchers do that?
Yes, the researchers took skin biopsies at the start and finish of the study. Given the effect that curcumin has been shown to have on alpha synuclein protein, the investigators wanted to evaluate levels of alpha synuclein in these skin cells.
What did they find?
They reported that levels of a specific form of alpha synuclein increased in the untreated group, but that increase was less in the curcumin-supplemented group. And interestingly, here the researchers observed that the decrease in alpha synuclein levels was larger in those on the treatment group with longer disease duration (no significant difference was found in alpha synuclein levels in those with short disease duration).
The researchers concluded their study by writing that their results “suggest that curcumin can cross the blood-brain barrier, that it is effective in ameliorating clinical parameters” and that there was a trend towards decreased alpha synuclein accumulation in the skin of treated individuals.
Now before we get too excited by these results, I would like to just quickly remind you that this was:
- A very small study – only 19 individuals being treated with curcumin
- Not a blinded study – everyone knew what they were being treated with (which means that there could have been a placebo response (a treatment-associated response that has no biological basis beyond the expectations of the participant)
Is this the only study investigating curcumin in Parkinson’s?
In terms of new formulations that improve the bioavailability of curcumin, no – this is not the only study.
In fact, just this month another study was published:
 Title: Evaluation of curcumin as add-on therapy in patients with Parkinson’s disease: A pilot randomized, triple-blind, placebo-controlled trial.
Title: Evaluation of curcumin as add-on therapy in patients with Parkinson’s disease: A pilot randomized, triple-blind, placebo-controlled trial.
Authors: Ghodsi H, Rahimi HR, Aghili SM, Saberi A, Shoeibi A.
Journal: Clin Neurol Neurosurg. 2022 Jul;218:107300.
PMID: 35636380
In this study, the researchers conducted a randomized, triple-blind, placebo-controlled, add-on study in which they recruited 60 participants and assigned them to treatment with either a nano-formulation of curcumin (to increase bioavailability) or a placebo.
They blindly followed these two groups for 9 months of daily treatment and…
…found no statistical differences in any of the clinical measures assessed. The researchers concluded their study by saying that “while curcumin is a well-tolerated natural compound, this trial was unsuccessful in showing its efficacy in quality of life and clinical symptoms“.
That said, they did see a trend in terms of MDS-UPDRS motor scores between groups suggesting a slight positive response (but it was not statistically significant).
And what is curious here is that this same group of researchers had previously published results of another study investigating this same formulation of curcumin in people with Parkinson’s. And in that study they had reported a positive response:
 Title: Effect of Nanomicelle Curcumin on Quality of Life and Sleep in Patients With Parkinson’s Disease: A Double-Blind, Randomized, and Placebo-Controlled Trial
Title: Effect of Nanomicelle Curcumin on Quality of Life and Sleep in Patients With Parkinson’s Disease: A Double-Blind, Randomized, and Placebo-Controlled Trial
Authors: Maghbooli M, Safarnejad B, Mostafavi H, Mazloomzadeh S, Ghoreishi A
Journal: Int Clin Neurosci J. 2019 Autumn;6(4):140-145
PMID: N/A
In this study, the researchers had recruited 50 individuals with Parkinson’s and and randomly assigned them into the curcumin or placebo treatment groups (25 each). They assessed sleep, fatigue, and quality of life over a 3 month period. They found that the curcumin treatment significantly increased sleep quality and quality of life (compared with the placebo), but it had no effect on overall fatigue.
If you ask me for my opinion (which I rarely give), I would argue that there is some encouraging data here, but larger and longer studies of curcumin in Parkinson’s are required.
And feel free to leave a comment in the comment section below if you agree/disagree.
|
# # RECAP #2: Slow release curcumin treatment has been found in clinical trials to have some beneficial effects in people with Parkinson’s. The slow-release formulation is used to improve bioavailability (spread and availability in the body). # # |
Have there been clinical studies of curcumin in other neurodegenerative conditions?
Yes there have.
And there have also been encouraging results here as well. Of particular interest to our discussion here today is a study that was reported several years ago. It involved another reformulation of curcumin (in nanoparticle form for better bioavailability – called Theracurmin) and the researchers tested it in non-demented adults:
 Title: Memory and Brain Amyloid and Tau Effects of a Bioavailable Form of Curcumin in Non-Demented Adults: A Double-Blind, Placebo-Controlled 18-Month Trial.
Title: Memory and Brain Amyloid and Tau Effects of a Bioavailable Form of Curcumin in Non-Demented Adults: A Double-Blind, Placebo-Controlled 18-Month Trial.
Authors: Small GW, Siddarth P, Li Z, Miller KJ, Ercoli L, Emerson ND, Martinez J, Wong KP, Liu J, Merrill DA, Chen ST, Henning SM, Satyamurthy N, Huang SC, Heber D, Barrio JR.
Journal: Am J Geriatr Psychiatry. 2018 Mar;26(3):266-277.
PMID: 29246725 (This report is OPEN ACCESS if you would like to read it)
In this study, the researchers conducted a double-blind, placebo-controlled study of a Theracurmin (which contained 90 mg of curcumin twice daily) in 40 non-demented adults (age 51–84 years). They randomly assigned the participants to either curcumin twice daily (N = 21) or placebo twice daily (N = 19) for 18 months. They then put all of the participants through a series of cognitive tests and conducted brain imaging assessments.
At 18 months, the researchers found that the Theracurmin-treated group had significantly improved their performance on many of the memory tests, compared to the placebo group (and remember that these were non-demented adults). As you can see in the graph below, the Theracurmin-treated group were 15 points better on the Buschke Selective Reminding Test (a verbal memory assessment) than the placebo group at the end of the study:
 Source: PMC
Source: PMC
In addition, the researchers reported that FDDNP-PET brain imaging of the participants at the start and end of the study suggested that the improvements in memory were associated with decreased accumulation of Alzheimer’s-associated beta-amyloid and tau protein in brain regions involved in mood and memory.
What is FDDNP-PET?
2-(1-{6-[(2-[fluorine-18]fluoroethyl)(methyl)amino]-2-naphthyl}-ethylidene)malononitrile (or FDDNP) positron emission tomography (PET).
Next question?
Just kidding.
FDDNP-PET is a method of visualizing signs of Alzheimer’s pathology (protein aggregates) in living humans. Specifically, it is used to locate beta-amyloid and Tau protein aggregates, typically in the brain (and no, it doesn’t detect Parkinson’s associated alpha synuclein).
So in this study, the researchers found that the improvements in memory that they observed in the participants treated with Theracurmin were associated with decreases in the levels of protein accumulation that were seen with the FDDNP-PET brain imaging.
The investigators of this study concluded their write up of the results by saying “Daily oral Theracurmin may lead to improved memory and attention in non-demented adults“.
Interesting. Has anyone tested this product in Alzheimer’s?
Yes, they have.
Last year this report was published:
 Title: Theracurmin Supplementation May be a Therapeutic Option for Older Patients with Alzheimer’s Disease: A 6-Month Retrospective Follow-Up Study.
Title: Theracurmin Supplementation May be a Therapeutic Option for Older Patients with Alzheimer’s Disease: A 6-Month Retrospective Follow-Up Study.
Authors: Dost FS, Kaya D, Ontan MS, Erken N, Bulut EA, Aydin AE, Isik AT.
Journal: Curr Alzheimer Res. 2021;18(14):1087-1092.
PMID: 34939543
In this study, the researchers conducted a six month study in 19 individuals with Alzheimer’s and 17 with “mild cognitive impairment” (or MCI). They were treated with 180 mg/day of Theracurmin. They compared the cognitive changes in these individuals over the 6 month period with 57 additional Alzheimer’s/MCI cases who acted as controls for the study.
After 6 months, the investigators found that the cognitive scores decreased (or got worse) in all of the participants not treated with theracurmin, while those same scores remained stable in the individuals treated with theracurmin.
So not an improvement, but a stablization at least.
Wow. I’m going to rush out and get me some Meriva or Theracurmin. Where can I get it from?
Before you do that (and yes, I am about to rain on the parade), there are some corners of the research community that express caution when we approach the idea of using curcumin as a therapeutic treatment. They are specifically concerned about the chemistry of curcumin and the strength of some of the supporting data.
Before discussing any self-experimentation with curcumin-associated products with your clinician, I would suggest reading this review of the field (SPOILER ALERT: it’s not very flattering, but it does back everything up with references and citations):
 Title: The Essential Medicinal Chemistry of Curcumin.
Title: The Essential Medicinal Chemistry of Curcumin.
Authors: Nelson KM, Dahlin JL, Bisson J, Graham J, Pauli GF, Walters MA.
Journal: J Med Chem. 2017 Mar 9;60(5):1620-1637.
PMID: 28074653 (this report is OPEN ACCESS if you would like to read it)
And to be fair, there have been responses to this report which take up other positions regarding curcumin (Click here to read one such example).
So what does it all mean?
I find curcumin rather frustrating.
It is is one of those supposedly ‘miracle’ agents that has been around forever and a day, but there has never been a proper clinical test of it – at scale, statistically well-powered, over a reasonable enough period of time – to determine if it actually lives up to the hype. The studies we have reviewed in this post today were probably adequate in terms of treatment time (12 to 18 months), but they each had other weaknesses (such as low number of participants). It is a shame really, as there seems to be hints of some thing happening.
You may think I am being overly skeptical, but this is the best approach. Until carefully controlled confirmatory data is presented, expectations must be managed and all biases removed.
We’ll keep an eye out here at SoPD HQ for more studies like these, and report them as their results become available.
 All of the material on this website is licensed under a
All of the material on this website is licensed under a
Creative Commons Attribution 4.0 International License
You can do whatever you like with it!
EDITOR’S NOTE: The information provided by the SoPD website is for information and educational purposes only. Under no circumstances should it ever be considered medical or actionable advice. It is provided by research scientists, not medical practitioners. Any actions taken – based on what has been read on the website – are the sole responsibility of the reader. Any actions being contemplated by readers should firstly be discussed with a qualified healthcare professional who is aware of your medical history. While some of the information discussed in this post may cause concern, please speak with your medical physician before attempting any change in an existing treatment regime.
This post involves commercially available products. At the time of writing, the author of this blog had had no recent contact (within the last 2 years) with any individuals associated with the companies or connected parties, nor has he benefited in any way from writing this post. This post does not represent an advertisement or endorsement of any of the products. The author was simply interested in some of the recently published results of the clinical studies presented and wanted to share them here in order to generate discussion.
The banner for today’s post was sourced from FB


Simon, It has long been known that “vitamin”D3 promotes expression of Nrf2 and that most humans are low on D3 by physiological criteria. One of those criteria is the serum 25(OH)D3 that is ca 100-150nmol/L in rural-dwelling Kenyans. Sporadic PD is absent in elderly rural Kenyans. I dont know how much curcumin they consume, but few of us in the urban world – and in the curcumin trials I guess- will reach even half their serum 25(OH)D. My serum level in 125 nmol/L and it takes 4000 IU pd to attain that, as a supplement. I’ll pass on curcumen, D3 does lots besides promoting Nrf2….. Peter
LikeLike
Thank you for all you do Simon! I have a question about the “The Effect of Curcumin on Idiopathic Parkinson Disease: A Clinical and Skin Biopsy Study” please:
It’s about the “The Curcumin Effect on Pathological Form of α-Syn in Skin Nerves”. The way I read this section is the treated group had an actual reduction in p-syn from baseline to 12 months. Not a decreased rate of increase, but an actual decrease (not a great amount of decrease, but a decrease. As opposed to the untreated group, that had an increase in p-syn).
Am I reading this wrong? Thanks, Dave
LikeLike